
Demographics are steadily shifting towards an aging population, worldwide; by 2050, it is estimated that 25% of the global population will be of advanced age.1 Such knowledge should behoove one to preemptively consider interventions to manage health. In this author’s previous posts, information was provided regarding advanced age (i.e., 65+), sarcopenia, and general interventions to manage degradation of muscle mass, strength, and physical performance. In the following sections, this author will consider specific recommendations as they relate to exercise selection, exercise type, and why such exercises are integral to managing sarcopenia.

As a means of briefly recapping, a central factor in managing sarcopenia is increasing force production/strength via increased muscle mass.2 Additional evidence has suggested that 20-30 minutes (time) of resistance training 2-3 times per week (frequency) had favorable effects upon sarcopenia.2(360) Such effects included increases in muscle volume and rapid increases in strength during the first few weeks of exercise, suggesting that strength can improve relatively quickly.2(360) Other key recommendations included incorporating 8-12 repetitions, 3 sets per exercise at an intensity of 60-80% of a one-repetition maximum.2(361)
As a reminder, although a plethora of exercise choices exist for elderly individuals, it is paramount that exercise professionals working with said population perform a functional movement screen (FMS) first; it assesses the mobility and stability of joints, muscles and basic movement/developmental patterns of the body. It allows one to see if a person’s musculoskeletal system is ready to safely withstand loads required to develop strength in functional/everyday movements (i.e., pushing, pulling, lifting, squatting, carrying, and locomotion) while helping direct exercise progressions in a safe and efficacious manner. The FMS also allows one to track change, progress, and uncover faulty patterns which may cause/contribute to muscular discomfort and pain. Please click on the following links for more information:
My Use of the Functional Movement Screen
Movement Dysfunctions and Assessment Techniques
The Joint-By-Joint Approach: A Road Map to Movement Dysfunctions

Although resistance training can be achieved largely via free weights (FWs) and machine-based exercise (MBE), similarities, and differences, are present between said interventions. FWs and MBEs were found to induce similar increases in muscle thickness and strength.3 From such a standpoint, both approaches could help elderly individuals achieve increases in force production. However, FW are likely to offer a unique advantage by improving joint stability.3(1858) Joint stability can be defined by physiological processes, which maintain optimal joint positions during static (i.e., staying still) and dynamic (i.e., moving) motions.
Optimal stability helps protect joints, muscles, tendons, and ligaments; characteristics unlikely to be achieved as robustly through MBEs when compared to FWs. Joint stability is largely governed (though not completely) by three processes; co-contraction, feed-forward/feedback control, and muscle recruitment patterns.4 As an aggregate, co-contraction/feed-forward, feedback/muscle recruitment patterns work in a highly coordinated and harmonious fashion to maintain and protect optimal joint positions during static and dynamic movement patterns. As a means of appreciating such processes and their relationship to FWs, the following will explore the constituents of stability in greater detail.
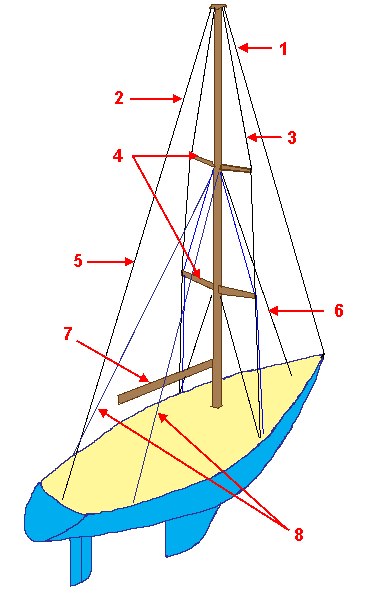
Co-contraction can be thought of as multiple muscles surrounding a joint (i.e., stabilizer muscles), activating together to induce joint compression and stiffness.4(355) An analogy that might clarify such a concept would be multiple support cables (similar to muscles) of similar tension surrounding a sail boat mast to maintain its upright position. Feed-forward/feedback control emanates from the neuromuscular system; a network of nerves sending and receiving information to stabilizer muscles (as well as to prime movers). Ideal signaling to and from the nervous system (i.e., feed-forward/feedback control) to stabilizer muscles around a joint help induce optimal recruitment and timing (the final characteristic of stability) of the same.4(355) Recruitment and timing relates to the number of muscle fibers stimulated and how quickly they activate, respectively. Optimal joint stability is characterized by early and successful activation of muscles.4(355)

Use of FWs and its relationship to joint stability is further supported by the research of Schwanbeck et al.3(1858) During their experiment, subjects that implemented FWs had a substantially higher degree of muscle recruitment when compared to MBEs, assessed via electromyography.3(1858) FWs also demand a higher degree of balance when conducting exercise, which can be defined as the ability to maintain an upright posture during static and dynamic motions.3(1858),5 Considering most MBEs have individuals in seated positions, it is unlikely balance is sufficiently accessed, stimulated, or challenged. However, FWs are inherently versatile allowing use in supine, prone, tall kneeling, half kneeling, split stance, standing, walking, and jumping positions.
In conclusion, demographics are steadily shifting towards an aging population, worldwide; by 2050, it is estimated that 25% of the global population will be of advanced age. Such knowledge demands that exercise professionals, and aging individuals, consider interventions that manage sarcopenia in a safe and systematic fashion. Strength and stability training, as part of a larger and more robust set of interventions, can help manage the deleterious effects of muscle and strength losses. Ultimately and most relevently, said approaches have the capacity to improve and protect the health, performance, and longevity of the elderly.
References
1. Di Lorito C, Long A, Byrne A, et al. Exercise interventions for older adults: A systematic review of meta-analysis. J Sport Health Sci. 2021;10(1):29-47. doi:10.1016/j.jshs.2020.06.003.
2. Mayer F, Scharhag-Rosenberger F, Carlsohn A, et al.: The intensity and effects of strength training in the elderly. Dtsch Arztebl Int. 2011;108(21):359–64.
doi:10.3238/arztebl.2011.0359.
3. Schwanbeck SR, Cornish SM, Barss T, et al. Effects of training with free weights versus machines on muscle mass, strength, free testosterone, and free cortisol levels. JStrength Cond Res. 2020;34(7):1851-1859. doi:10.1519/JSC.0000000000003349.
4. Sangwan S, Green RA, Taylor NF. Characteristics of stabilizer muscles: A systematic review. Physiother Can. 2014;66(4):348-358. doi:10.3138/ptc.2013-51.
5. Thomas E, Battaglia G, Patti A, et al. Physical activity programs for balance and fall prevention in elderly. Medicine. 2019;98(27):1-9. Doi:10.1097/MD.0000000000016218.
-Michael McIsaac
