
Physical function may be thought of as goal-directed movement, considered the link between physical actions, colloquially defined as movement, and the environment in which it takes place (Cech & Martin, 2012). Such characteristics are essential, as they permit individuals to survive, adapt, and learn within the environment (Cech & Martin, 2012).
If movement is inhibited or dysfunctional, an individual may be less able to participate in goal directed movement, in a meaningful and efficient manner. A key to mitigating movement impairment is through understanding the nature and purpose of the sensorimotor system. The following will consider movement impairment, using scapular dysfunction as an example, while exploring constituents of the sensorimotor system, and how it can impede shoulder stability.
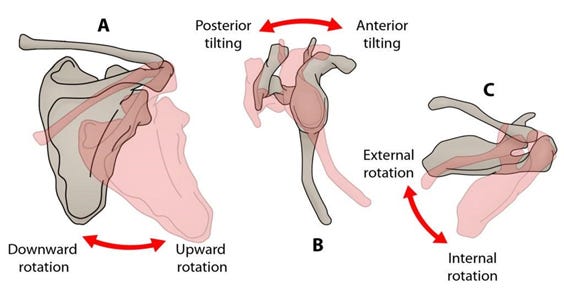
Scapular mobility, and stability, are considered requisites for successful and efficient glenohumeral motions; the scapula must act as an anchor for the glenohumeral joint, while stabilizing itself in a 3-dimensional motion (McClure, Greenberg, & Kareha, 2012). During arm motion, orientation of the scapula can be described through 3 positions: upward/downward rotation, anterior/posterior tilting, and internal/external rotation (McClure et al., 2012).
Consider arm elevation for example; there is a pattern of scapular upward rotation, posterior tilting, and external rotation, in addition to clavicular elevation and depression (McClure et al., 2012). All of the aforementioned motions must occur in a synchronized fashion, driven by the sensorimotor system, to develop dynamic stability, while the humorous is in motion.
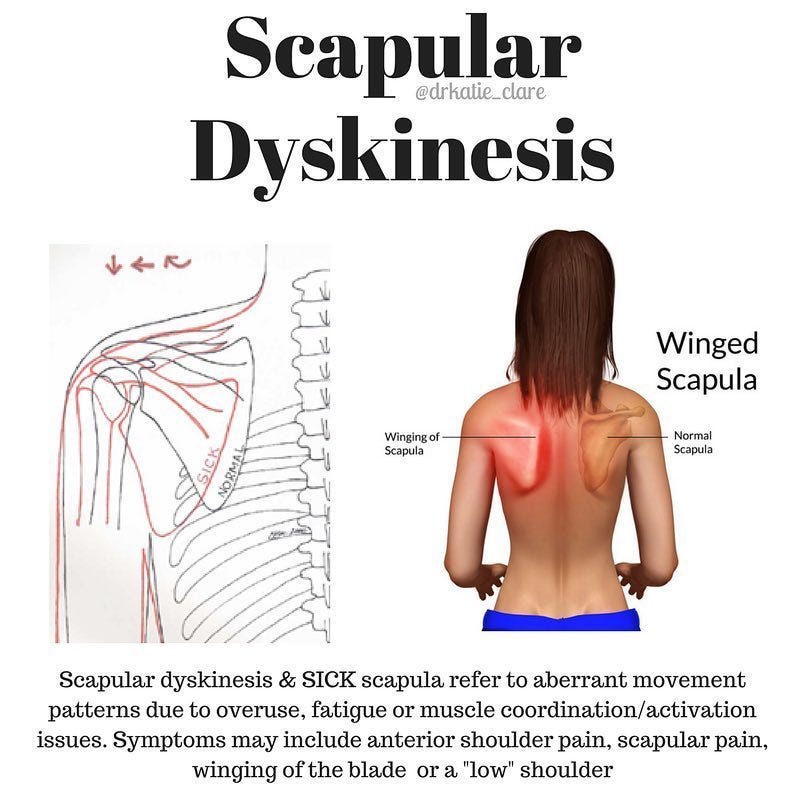
Scapular dyskinesis (SD) can be defined as alterations of scapular motions and positions during static and dynamic glenohumeral (GH) movements (Huang, Ou, Huang, & Lin, 2015). Although not all individuals with shoulder disorders exhibit dyskinesis, as many as 68%-100% of those with GH instability, rotator cuff tears, and labral tears do demonstrate aberrant scapular motions. Huang et al. (2015) explored SD with 82 subjects as a means of documenting atypical scapular movements.
Huang et al. (2015) classified scapular positions (i.e., during arm elevation in the scapular plane) as abnormal single pattern (inferior angle prominence, pattern I; medial border prominence, pattern II; excessive/inadequate scapular elevation or upward rotation, pattern III), abnormal mixed patterns, or normal pattern (pattern IV). Surface electrodes (i.e., electromyography) were also used to document muscle activity in each scapular orientation. Compared to a control group performing arm lowering, Huang et al. (2015) found several interesting results:
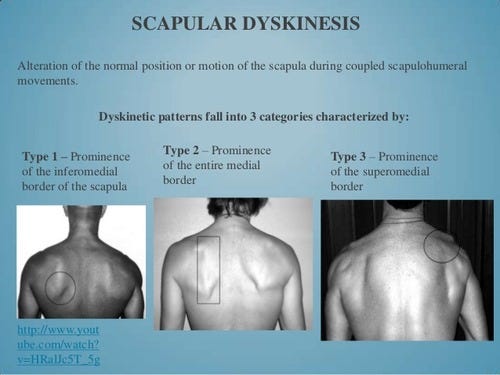
More scapular internal rotation was found in pattern II subjects and mixed pattern I and II subjects than in control subjects during arm lowering, scapular posterior tipping was less in pattern I subjects during arm lowering, higher upper trapezius activity was found in pattern II subjects during arm lowering, and serratus anterior and lower trapezius activity were less in mixed pattern I and II subjects during arm lowering.
The aforementioned results demonstrate that aberrant firing patterns (i.e., from an impeded sensorimotor system) are dependent upon the particular form of scapular dyskinesis presented by the subject. Neuromuscular control, defined as the unconscious activation of muscle stabilizers to prepare for and respond to joint movement, becomes hampered, causing poor shoulder stability and scapular tracking about the thorax (Page, Lardner, & Frank, 2010). Such uniqueness of firing patterns should serve as a reminder that exercises for scapular stability need to be specific to the scapular dysfunction, and that there may not be a “one size fits all” approach.
References
Cech, D., & Martin, S. (2012). Functional movement development across the lifespan (3rd ed.). St. Louis, MO: Elsevier Health Sciences.
Huang, T.S., Ou, H.L., Huang, C.Y., & Lin, J.J. (2015). Specific kinematics and associated muscle activation in individuals with scapular dyskinesis. Journal of Shoulder and Elbow Surgery, 24, 1227-1234.
McClure, P., Greenberg, E., & Kareha, S. (2012). Evaluation and management of scapular dysfunction. Sports Medicine and Arthroscopy Review, 20(1), 39-48.
Page, P., Lardner, R., & Frank, C. (2010). Assessment and treatment of muscle imbalances: The Janda approach. Champaign, IL: Human Kinetics.
-Michael McIsaac
