
Sleep quality/duration and nutrition are cornerstones of health and overall quality of life. Sleep is a vital, yet often, underappreciated component of homeostasis and in many westernized nations individuals tend to experience less hours of sleep per night.1 Sleep restriction of seven hours or less has been associated with longer work schedules and greater time associated with leisure activities.1(148) Ultimately, such widespread loss of sleep, and poor nutrition, has been associated with several conditions including coronary heart disease, diabetes, and of particular relevance, lowered immune function.1(148)2 As a means of appreciating the influence of sleep restriction and nutrition upon immune system strength/wound healing, the following will consider both in greater detail.
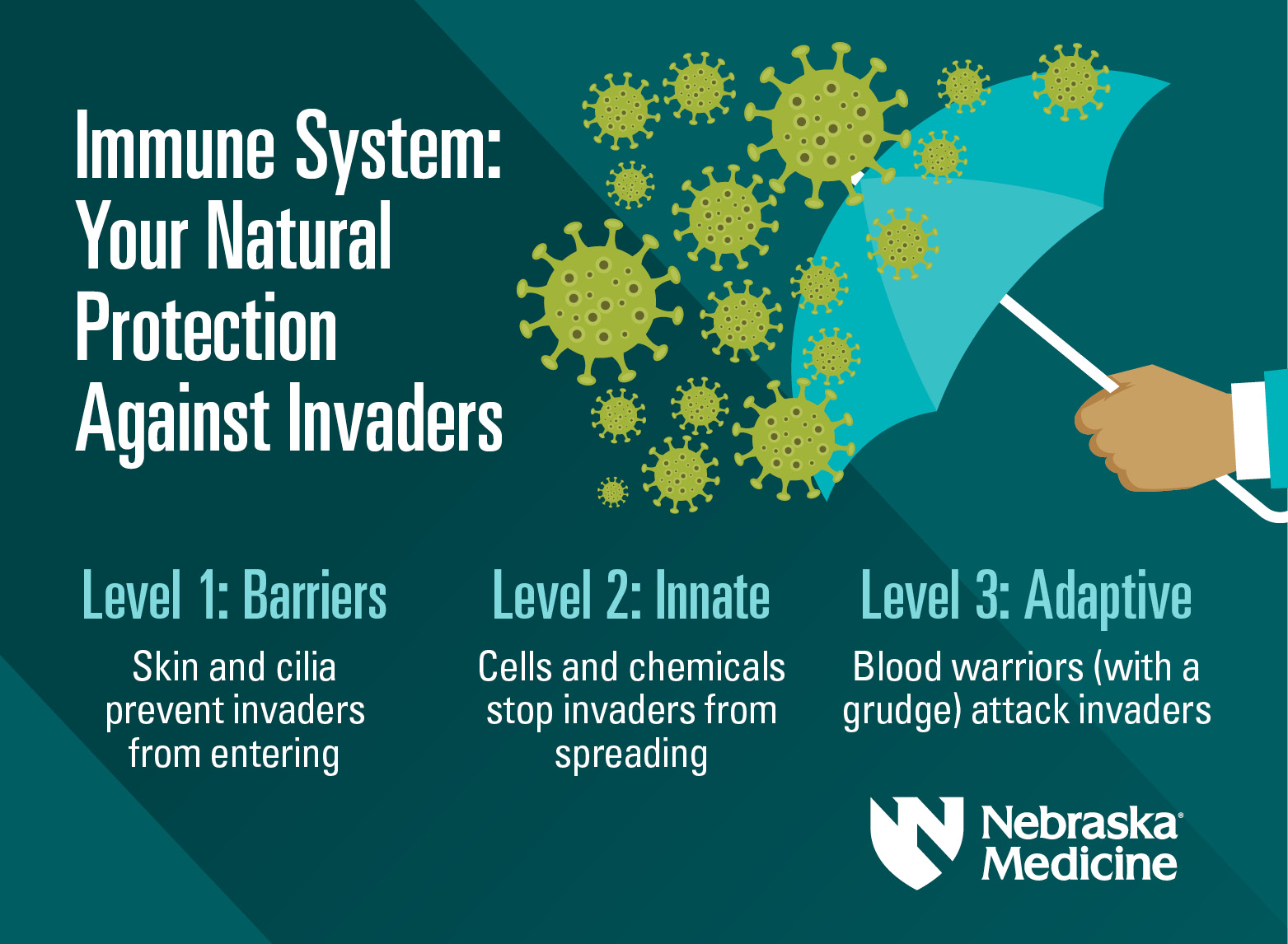
The immune system is a highly coordinated cascade of biochemical and physiological events that manage tissue injury from physical agents, chemical agents, and pathogenic organisms.3 Such tissue injuries undergo defensive and regenerative processes via innate immunity (quick response to a predetermined array of chemical signals) and adaptive immunity (a slower response that changes based on novel intruding molecules).3(93) Ultimately, the innate immune system is expeditious in nature but cannot fully eradicate injurious agents. However, innate immunity does prime the adaptive immune system buying time for the adaptive system to respond as a second line, and highly effective, mechanism in host defense.3(108) As a unit, both systems work symbiotically to neutralize foreign agents and induce tissue healing.
An optimally functioning immune system, then, is crucial in maintaining the health of individuals. Thus, any aberrations within the immune system response is likely to induce undesirable, and potentially fatal, effects upon the organism. Sleep restriction has been found to be a progenitor, among others, of compromised immune responses. Smith et al2(190) indicated that the effect was mediated by sympathetic nervous system /hypothalamic-pituitary-adrenal axis activation, and characterized by lowered natural killer cell activity, lowered interleukin-2 (stimulates immune response) production, with elevated proinflammatory cytokines (inflammatory molecule signalers).2(190) Such poor sleep hygiene, then, induces physiological events well beyond sensations of fatigue and poor cognition; the most common complaints noted by individuals.
Sleep restriction has been found to increase the risk of acquiring the common cold; individuals who experienced less than 6 hours of sleep per night were approximately four to five times more likely to contract a cold. Conversely, individuals who slept more than 7 hours a night were considerably less likely to acquire the cold.2(190) In addition to adequate sleep, optimal immune function also requires several nutrients. For example, vitamin C helps in capillary function, collagen formation, neutrophil activity, and fibroblast proliferation.2(190) Omega-3 fatty acids enhance natural killer and T-cell activity, which reduces inflammation. Arginine contributes to cellular growth, and collagen deposition, while glutamine initiates the proliferation of fibroblasts and wound healing.2(190) Thus, deficits in sleep quality and nutrition can induce unfavourable changes in immune function, response time, and wound healing.
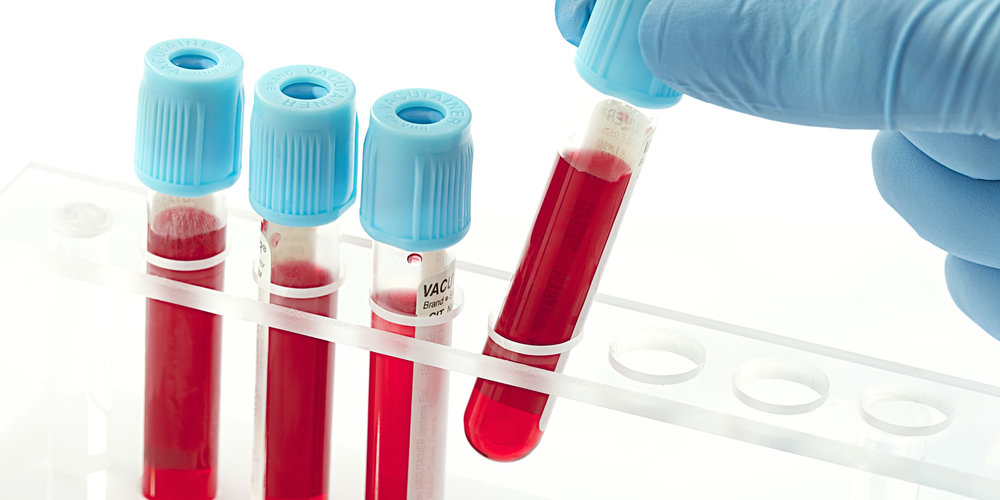
Circulating blood markers of immune function help assess the systemic immune response, however, such markers do not fully elucidate functional status, or the ability to heal from a wound or fight against an infection.2(191) In contrast, wound healing models, like the suction blister model, directly assess functional status of wound healing (i.e., innate immune response) which also tends to provide insights on local proinflammatory responses and tissue remodeling processes.2(191)Such a test acts as a proxy measure of wound healing rate, and ultimately, immune system function. As a means of appreciating the influence of sleep and nutrition upon would healing/immune system strength, the following will outline a study conducted by Smith et al2(191) whereby sleep restriction and would healing rate was assessed (phase 1), as well as nutritional protocols and rate of wound healing (phase 2).
56 participants were included in the study, were between the ages of 19-35 years, considered generally healthy, sleeping 7-9 hours sleep per night before the experiment, and not taking medications.2(192) In phase 1, the degree of short-term sleep restriction (3 days of sleep restriction with 2 hours of sleep per night) on immune response and skin barrier healing at the wound site was assessed by comparing sleep-restricted participants to free-living participants with adequate sleep.2(191) Phase 2 was characterized by the use of a multinutrient supplement (L-arginine, L-glutamine, omega-3 fatty acids, zinc sulfate, vitamin D3, and vitamin C) and a diet providing 1.5 g protein/kg during, and after, sleep restriction.2(191) The goal was to determine if nutritional interventions and conditions attenuated decrements in local immune function and skin barrier restoration observed, especially amongst sleep-restricted individuals, when compared to a diet providing 0.8 g protein/kg bodyweight combined with a placebo beverage during, and after, sleep restriction.2(192)
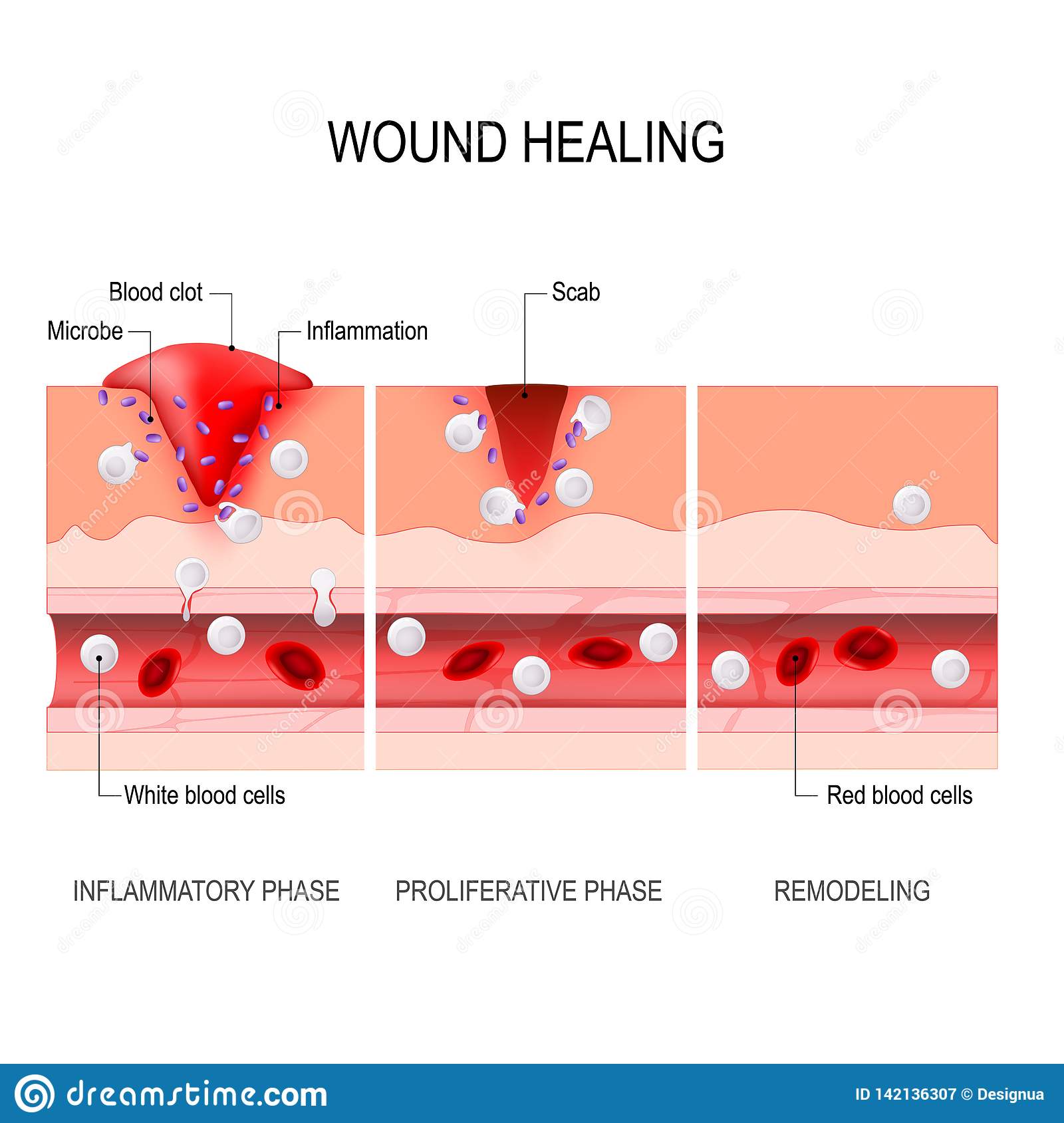
Results from the study indicated that sleep restricted groups experienced significantly longer wound healing times (~5 days) compared to individuals who received adequate sleep (~4.2 days). Furthermore, proinflammatory cytokines at the wound region were elevated during the initial phase of healing for the high protein/multinutrient beverage participants (during and after sleep restriction conditions) compared with participants who received a lower protein intake with placebo beverage under the same sleep restriction conditions. Interestingly, despite the presence of higher pro-inflammatory cytokines in the high protein/multinutrient group, the rate of wound healing was the same between both high protein/multinutrient and low protein/placebo multinutrient intake protocols.2(197) However, the higher protein group did experience greater levels of pro-inflammatory cytokines, which may help maintain immune system strength despite a lack of improvement in wound healing rates.
In conclusion, sleep quality/duration and nutrition are cornerstones of health and overall quality of life. Sleep is a vital, yet often, underappreciated component of homeostasis and in many westernized nations individuals tend to experience less hours of sleep per night. Sleep restriction has been shown to lower wound healing rates in the presence, and absence, of higher protein/multinutrient diets. Ultimately, said research should remind individuals of the influence of sleep duration and its impact upon immune system integrity. Finally, it is this author’s hope that such knowledge will encourage individuals to seek improved sleep hygiene as another means of maintaining and protecting health and overall quality of life.
References
1. Gallicchio L, Kalesan B. Sleep duration and mortality: A systematic review and meta-analysis. J Sleep Res. 2009;18:148-158. doi:10.1111/j.1365-2869.2008.00732.x.
2. Smith TJ, Wilson M, Karl JP, et al. Impact of sleep restriction on local immune response and skin barrier restoration with and without “multinutrient” nutrition intervention. J Appl Phys. 2017;124(1):190-200. doi:https://doi.org/10.1152/japplphysiol.00547.2017.
3. Reisner EG, Reisner HM. An Introduction to Human Disease: Pathology and Pathophysiology Correlations. 10 th ed. Burlington, MA: Jones & Bartlett Learning; 2017.
-Michael McIsaac
