Small intestinal fungal overgrowth (SIFO) is a condition defined by an excessive concentration of fungal microorganisms inhabiting the small intestine (SI). Such a condition is often found amongst immunocompromised individuals or those who use antibiotics with symptoms ranging from belching, indigestion, bloating, diarrhea (leading to nutrient deficiencies), nausea, and gas (Erdogan & Rao, 2015). However, recent evidence has suggested SIFO also exists among individuals with healthy immune function and its genesis is thought to derive from a lack of motility and/or antacid use (Erdogan & Rao, 2015). The following will consider SIFO, its causes, and solutions in greater detail.
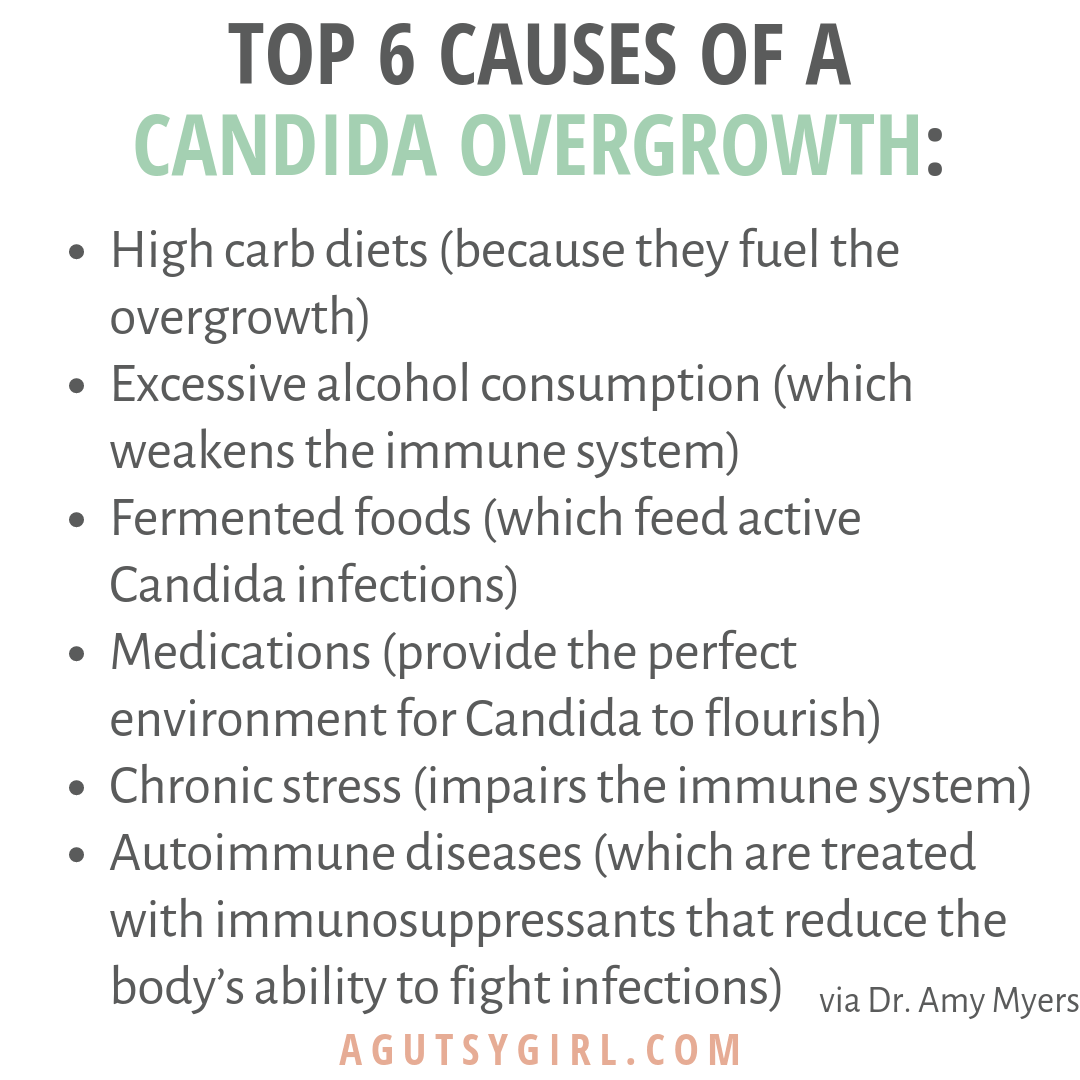
SIFO is largely characterized by overgrowth of a specific fungus known as Candida; a typically opportunistic microorganism colonizing the skin and mucosal surfaces of the body (Erdogan & Rao, 2015). Generally, innate and adaptive immunological processes control the levels of fungus along the SI. Furthermore, other species of bacteria facilitate control of fungal overgrowth to include Lactobacillus species by producing hydrogen peroxide (Erdogan & Rao, 2015). However, any damage to the mucosal barrier of the SI or microbiome (i.e., chemotherapy, antibiotics, inflammatory processes, immune molecule activation, and epithelial repair disruption) may provide fertile grounds for SIFO (Erdogan & Rao, 2015). Thus, an optimally functioning SI is central to maintaining normal fungal populations.
Erdogan and Rao (2015) stated that other protective mechanisms exist to prevent SIFO to include gastric acid and pancreatic enzymes. Specifically, pancreatic enzymes have fungistatic (inhibiting the growth of fungi) capabilities while low pH stomach acid kills microbes inhibiting the growth of bacteria and fungus (Erdogan & Rao, 2015). Such knowledge helps support the strong association between SIFO and proton pump inhibitors (reduce stomach acidity/increase pH). If SIFO has been diagnosed via aspiration and culture of the duodenum/jejunum and organic acid testing through analysis of D-arabinitol levels, several protocols exist to manage such overgrowth (Erdogan & Rao, 2015; Lord & Bralley, 2012). The following will explore the same.

Erdogan and Rao (2015) indicated that SIFO intervention options are determined by the severity of the disease, history of tolerance/intolerance to antifungal therapy, involvement of other organs, underlying immune system function, and past exposure to pharmaceutical drugs. If antifungal medication is warranted, several types exist to facilitate concentrations of fungus to include azoles, nystatin, echinocandins, and antibiotics (Erdogan & Rao, 2015). Concurrent interventions to control SIFO might also include reduction in carbohydrate load, since SIFO can proliferate in its presence (Lord & Bralley, 2012). If individuals were on proton pump inhibitors, implementation of acidic liquids, foods, and/or hydrogen chloride (HCL) supplementation can help return pH to normal levels (Pizzorno & Katzinger, 2012).Finally, use of pancreatic enzymes can also facilitate appropriate digestion and help control fungal overgrowth (as stated in the previous section) (Lord & Bralley, 2012).
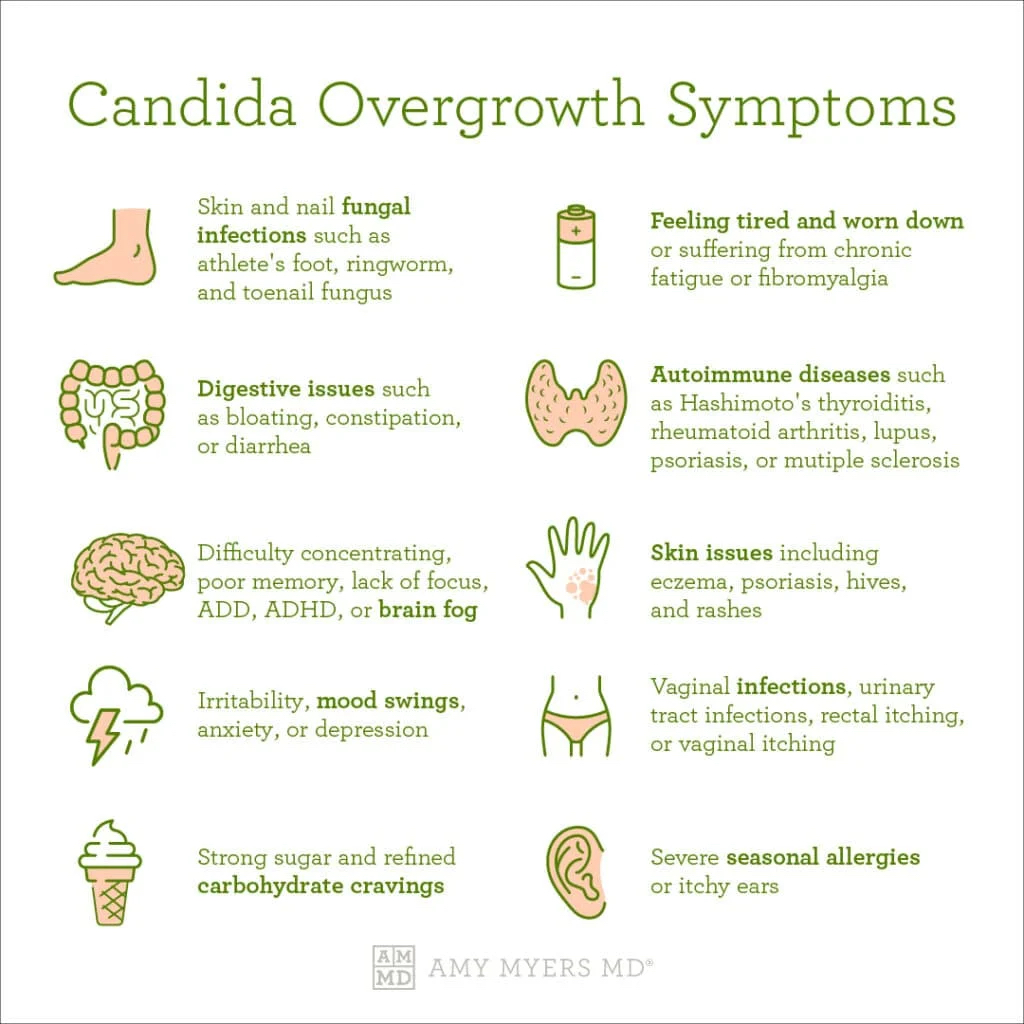
In conclusion, SIFO is a condition defined by an excessive concentration of fungal microorganisms inhabiting the SI. Immunocompromised individuals and those using antacids and antibiotics may present with symptoms ranging from belching, indigestion, bloating, diarrhea, nausea, and gas (Erdogan & Rao, 2015). Left unchecked, SIFO may lead to micronutrient deficiencies from excessive diarrhea (if present) and overloading of detoxification pathways from toxin production (Lord & Bralley, 2012). As such, it is imperative to recognize symptoms, and if present, follow-up with organic acid testing and/or aspiration and culture of the duodenum/jejunum. If SIFO is present, evidence suggests the use of pharmaceutical and nutritional interventions to reduce/mitigate said condition.
References
Erdogan, A., & Rao, S. S. C. (2015). Small intestinal fungal overgrowth. Current Gastroenterology Reports, 17(4), 1-7.
Lord, R. S., & Bralley, J. A. (2012). Laboratory evaluations for integrative and functional medicine (2nded.). Duluth, GA: Genova Diagnostics.
Pizzorno J. & Katzinger, J. (2012). Clinical pathophysiology: A functional perspective. Coquitlam, BC: Mind Publishing Inc.
-Michael McIsaac
