One hundred years ago, processed foods were minimal, mostly in the form of alcohol and breads. In the present day, societies contain many forms of processed products. Moreover, processed food is a dominant form of sustenance both in high-income and middle-income countries such as the United States (Monteiro, Moubarac, Cannon, Ng, & Popkin, 2013).
With processed foods came large portions of salts, sugars, and preservatives; compounds once minimal in both individuals and western culture (Monteiro et al., 2013). Processed foods also contain high levels of omega-6 fatty acids, which are molecules that can mount a constant low-grade immune response within the body. This author has written posts about omega-6 fatty acid immune responses in another course. An excerpt of said post is below:
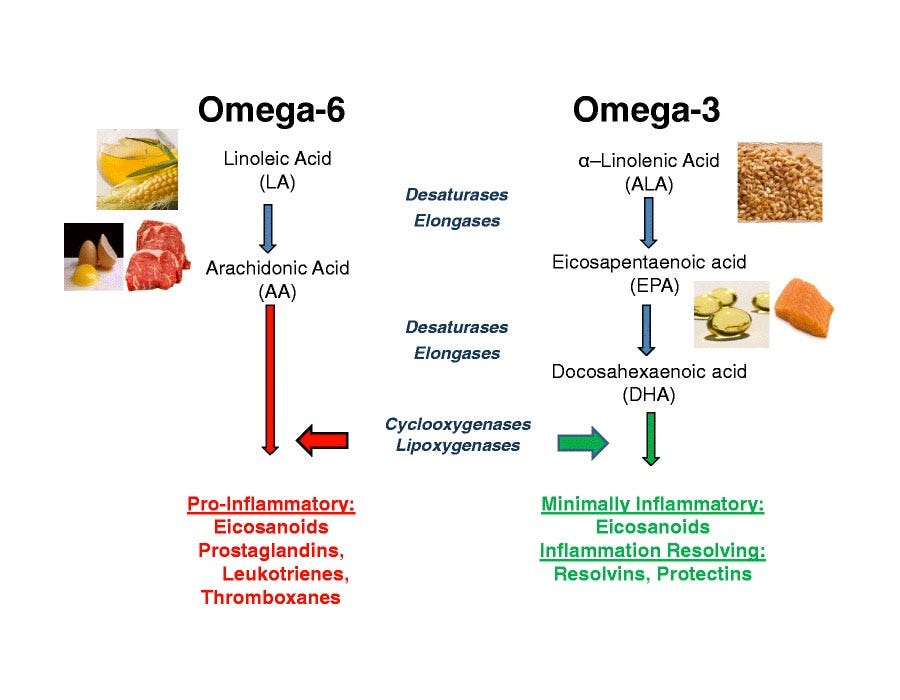
Briefly, omega-6 and omega-3 PUFAs undergo a biochemical change once absorbed. The metabolic products of both PUFAs include eicosanoids; signaling molecules responsible for the control of immune and inflammatory reactions in the body. Pro-inflammatory Omega-6 eicosanoids include prostaglandin E2, leukotriene B4, and thromboxane A2. Eicosanoids are generated by the enzymes lipoxygenase-5 and cyclooxygenase-2 (Ilich et al., 2014). Omega-3 eicosanoids, which are anti-inflammatory in nature, include prostaglandin E3, leukotriene B5, resolvins and protectins.
Here, anti-inflammatory eicosanoids also use lipoxygenase-5 and cyclooxygenase-2 (Ilich et al., 2014). Of particular relevance and interest are the shared enzymes between the two PUFAs (i.e., lipoxygenase-5 and cyclooxygenase-2); both PUFAs compete for use of lipoxygenase-5 and cyclooxygenase-2. Thus, if more omega-6 fatty acids are present in the diet than omega-3 fatty acids, more pro-inflammatory signaling molecules are created, and larger levels of systemic inflammation will occur.
If chronic consumption of high omega-6 / omega-3 ratios continue, chronic systemic inflammation ensues (Ilich et al., 2014). An inflammatory response also produces cytokines such as tumor necrosis factor alpha, interleukin-6, and interferon-gamma; proteins important in cell signaling and immune responses (Ilich et al., 2014). Low-grade chronic inflammation (LGCI) from overconsumption of omega-6 PUFAs perpetuates the production and levels of these pro-inflammatory signalling molecules.

There are also possible addictive qualities of refined carbohydrates (Ifland et al., 2009). If such a submission is true, it would help provide greater insight regarding the origins of metabolic syndrome, and the challenges of removing processed carbohydrates from the diet. Ifland et al. (2009) hypothesized that processed foods possessed an aggregate of substances that were addictive: refined sugar, sweeteners, other refined carbohydrates (i.e., flours), fat, salt, and caffeine, which are not naturally found in nature in one food.
Such a proposal could provide a plausible explanation for overeating. Ifland et al. (2009) also noted that over the past forty years, there has been a paralleled increase in refined carbohydrate consumption and metabolic syndrome. Such knowledge helps one appreciate why many obese individuals find it difficult to remove said food type in the diet.
Obesity is also associated with gut dysbiosis. Microbiota can be defined as a collection of a variety of microbes, with over 1000 different species in the small intestine alone. The collective genomic contents of microbiota are called the microbiome (Villanueva-Millán, Pérez-Matute, & Oteo, 2015).
Additionally, the microbiome plays essential roles in the maintenance and development of the immune system, metabolism, and homeostasis in general (Villanueva-Millán et al., 2015). Thus, if the microbiome is compromised, so too will the aforementioned roles it participates in.
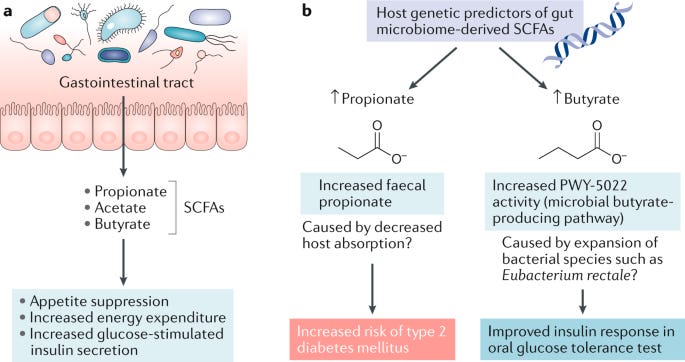
Of particular interest is the influence of gut micriobiota on the maintenance of bodyweight. Villanueva-Millán et al. (2015) noted that intestinal microbiota are involved in the development of short-chain fatty acids (SCFA). SCFAs, once absorbed through the intestinal wall, are associated with an increase in satiety and a reduction in food intake in the individual. Thus, properly functioning microbiota are instrumental in appetite control and fat-free mass. The researchers also indicated that SCFAs induce the expression of leptin (suppresses hunger) in adipose tissue, another potential mechanism of modulating appetite and body weight (Villanueva-Millán et al., 2015).
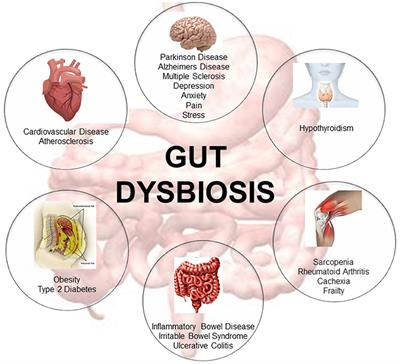
In obese individuals, however, there were aberrations in the relative abundance and ratios of different bacteria (Villanueva-Millán et al., 2015). More specifically, the researchers indicated that changes in specific bacteria and diversity were likely to be the most important factors rather than general changes in bacteria as a whole (Villanueva-Millán et al., 2015). Such gut dysbiosis has been associated with the intestine over-absorbing calories and limiting fat oxidation in the obese, furthering weight gain. Thus, a properly functioning microbiome is paramount in maintaining lean body mass.
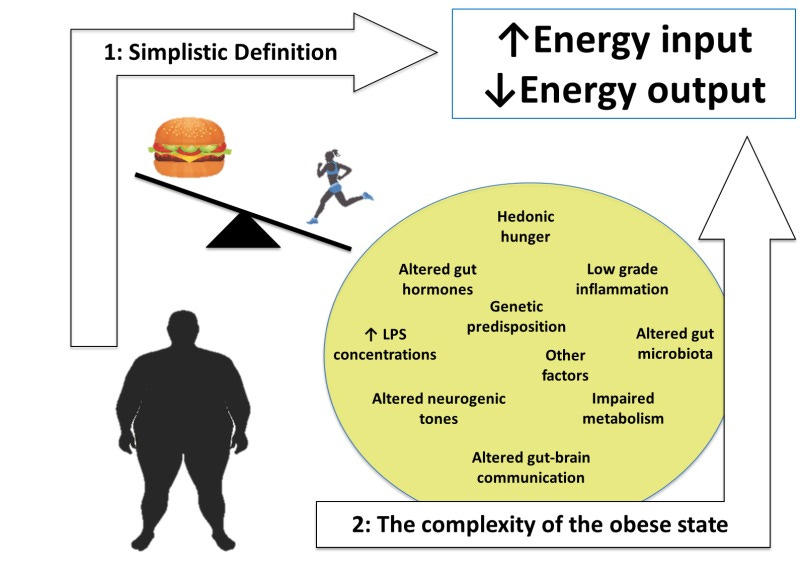
In conclusion, obesity cannot simply be mitigated by overly simplistic approaches as “exercise more” or calling it a disease. There are cultural proclivities, changes in food production, apparent addictive qualities of processed foods, and aberrations in the gut microbiome that all contribute to such an epidemic, yet share intimate connections with each other and individuals’ lifestyle choices. In essence, obesity serves as the consummate example whereby a holistic approach is not only thoughtful to use but necessary to incorporate. Exercise professionals must be cognizant of the complexity behind obesity and be prepared to refer out to other professionals (i.e., nutritionists, functional medicine doctors, psychologists) when and where appropriate.
References
Ifland, J.R., Preuss, H.G., Marcus, M.T., Rourke, K.M., Taylor, W.C., Burau, K., …Manso, G. (2009). Refined food addiction: A classic substance use disorder. Medical Hypotheses, 72, 518-526.
Ilich, J.Z., Kelly, O.J., Kim, Y., & Spicer, M.T. (2014). Low-grade chronic inflammation perpetuated by modern diet as a promoter of obesity and osteoporosis. Archives of Industrial Hygiene and Toxicology, 65(2), 139-148.
Monteiro, C.A., Moubarac, J.C., Cannon, G., Ng, S.W., & Popkin, B. (2013). Ultra-processed products are becoming dominant in the global food system. Obesity Reviews. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24102801
Villanueva-Millán, M. J., Pérez-Matute, P., & Oteo, J. (2015). Gut microbiota: a key player in health and disease. A review focused on obesity. Journal of Physiology and Biochemistry, 71(3), 509-525.
-Michael McIsaac
