As was mentioned in my last post, genetic, lifestyle, and environmental factors have been correlated to breast cancer and estrogen production. Said factors include: poor detoxification, environmental toxins (PCB’s, cadmium), genetic polymorphisms (specifically COMPT and CYP1B1) for breast cancer, a diet consisting of increased fat and protein and low fiber intake, lack of sleep, decreased vitamin D levels, decreased calcium levels, and a lack of exercise (Pizzorno & Katzinger, 2012). In the following sections, I would like to consider one factor, vitamin D, and its role in human health, breast cancer, and longevity.
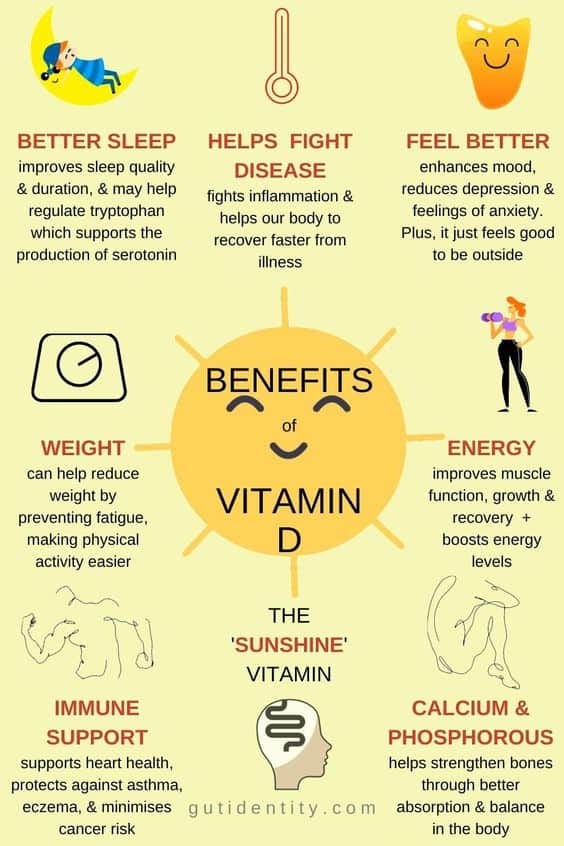
In the last decade, vitamin D has been shown to influence more than calcium turnover; vitamin D deficiency has been connected to several maladies including type 1 diabetes, multiple sclerosis, rheumatoid arthritis, inflammatory bowel disease, and overall cancer mortality (Gissel, Rejnmark, Mosekilde, & Vestergaard, 2008). Gissel et al. (2008) stated that in their meta-analysis study, females who ingested ≥400 IU/day of vitamin D yielded a homogenous result with a trend towards less breast cancer with ≥400 IU/day vs. the lowest intake (typically <50–150 IU/day). Thus, there might be a trend towards fewer cases of breast cancer with higher intakes of vitamin D (≥400 IU/day). Clearly, such a vitamin is essential to maintaining health, well-being, and longevity. Having considered vitamin D’s utility, the following will consider its subtypes and sources.

Vitamin D is comprised of a collection of molecules known as calciferols. The most common forms found in the human diet are cholecalciferol (vitamin D3), ergocalciferol (vitamin D2) and 25-hydroxyvitamin D (vitamin D3, found naturally in foods) (Bendik, Friedel, Roos, Weber, & Eggersdorfer, 2014). Another unique characteristic of vitamin D3 is its ability to be synthesized through the skin by sunlight, as well as through food intake (i.e., seafood such as seals, cod, herring, and mollusks); such a characteristic helps maximize the opportunities of vitamin D absorption (Chaplin & Jablonski, 2013). Thus, lack of sunlight and/or foods low in vitamin D can contribute to vitamin D deficiencies.
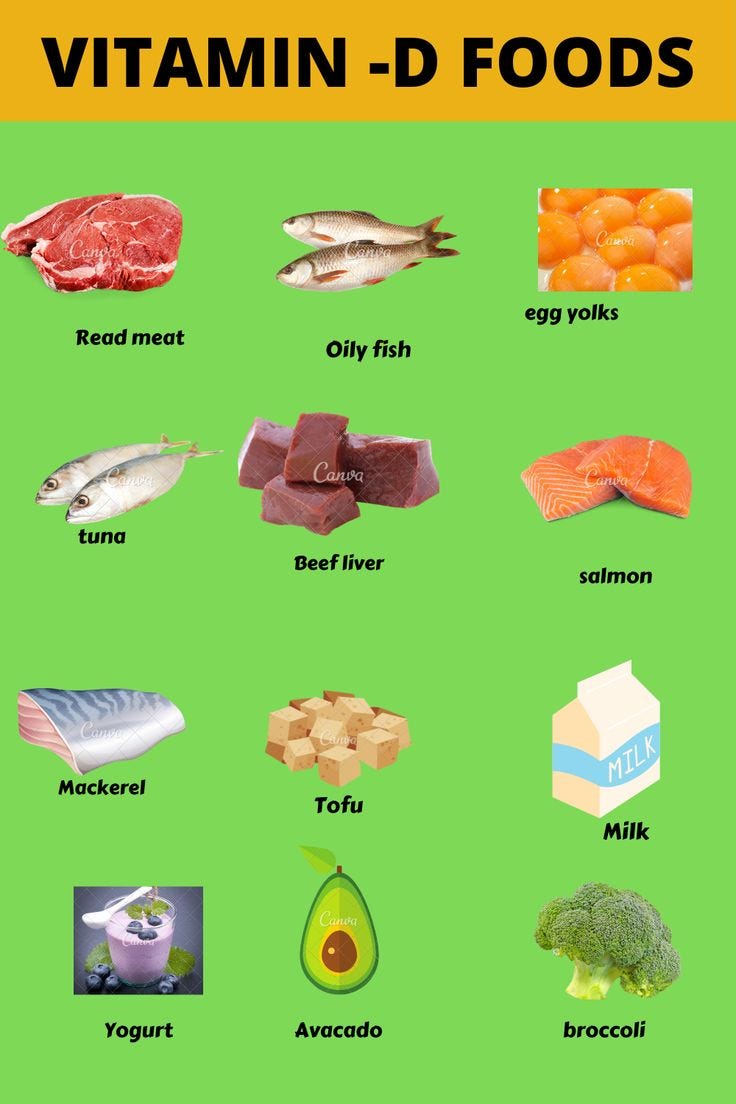
In conclusion, vitamin D has been implicated in several functions within the human body. Although deficiencies of vitamin D can negatively affect an individual, it is possible to regain normal levels through ingestion of natural foods, exposure to sunlight, in addition to supplementation. Although adequate vitamin D intake may not combat/prevent breast cancer as a stand-alone modality, it may complement a larger and more robust treatment intervention.
References
Bendik, I., Friedel, A., Roos, F., F., Weber, P., & Eggersdorfer, M. (2014). Vitamin D: A critical nutrient and essential micronutrient for human health. Frontiers in Physiology, 5, 1-14.
Gissel, T., Rejnmark, L., Mosekilde, L., & Vestergaard, P. (2008). Intake of vitamin D and risk of breast cancer- A meta-analysis. The Journal of Steroid Biochemistry and Molecular Biology, 111(3-5), 195-199.
Pizzorno J., & Katzinger, J. (2012). Clinical pathophysiology: A functional perspective. Coquitlam, BC: Mind Publishing.
-Michael McIsaac
