
Vitamin D is a micronutrient that has been associated with significantly reducing all-cause mortality, and has been implicated in many diseases of modern civilization (Cannell, 2008). Furthermore, and most relevantly, vitamin D interacts with more that 200 genes and multiple organs, indicating its broad reach and influence upon human physiology (Cannell & Hollis, 2008; Wang, Zhu, & DeLuca, 2012). Vitamin D, however, is a colloquial term used to describe several forms of said micronutrient: cholecalciferol (vitamin D3), calcidiol (25(OH)D), and calcitriol (1,25OH2D) with each having different functions. Additionally, measuring and determining optimal dosing vitamin D is critical due to its intricate and influential relationship with genes and cellular activity. As such, the following sections will explore the types, utility, screening, and dosing of vitamin D.
VITAMIN D RECEPTOR DISTRIBUTION
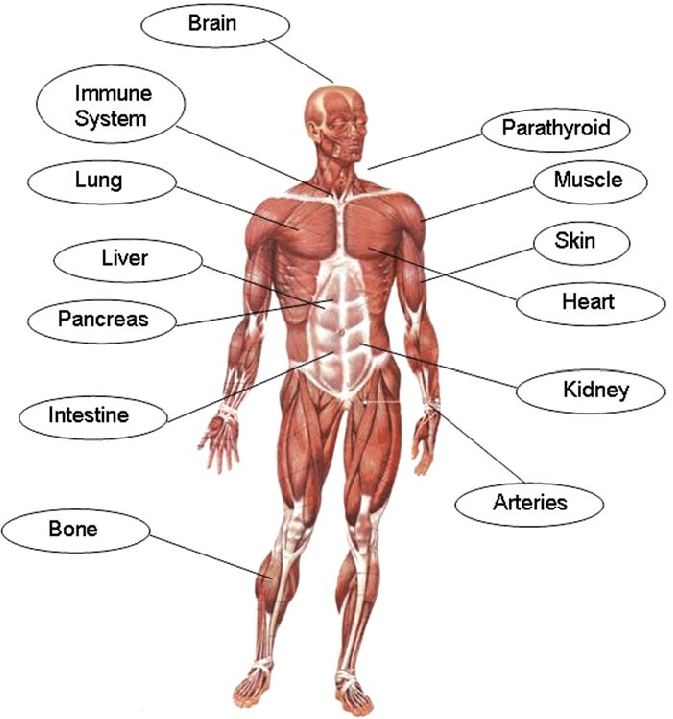
Vitamin D interacts with vitamin D receptor (VDR) sites within the intestinal epithelium, renal tubules, parathyroid gland cells, skin (keratinocytes), mammary epithelium, pancreas (beta islet cells), pituitary gland, skeleton (osteoblasts and chondrocytes), immune system (monocytes, macrophages, and T-lymphocytes), and germ tissues (Wang et al., 2012). The tissues with the highest VDR content are intestine, kidney, parathyroid gland, and bone, which are all involved in bone maintenance. Ultimately, such evidence is suggestive of the influence vitamin D has upon the body, and the requirement of said micronutrient. The following will consider the sources of vitamin D, as well as forms found within the body.
SOURCES OF VITAMIN D
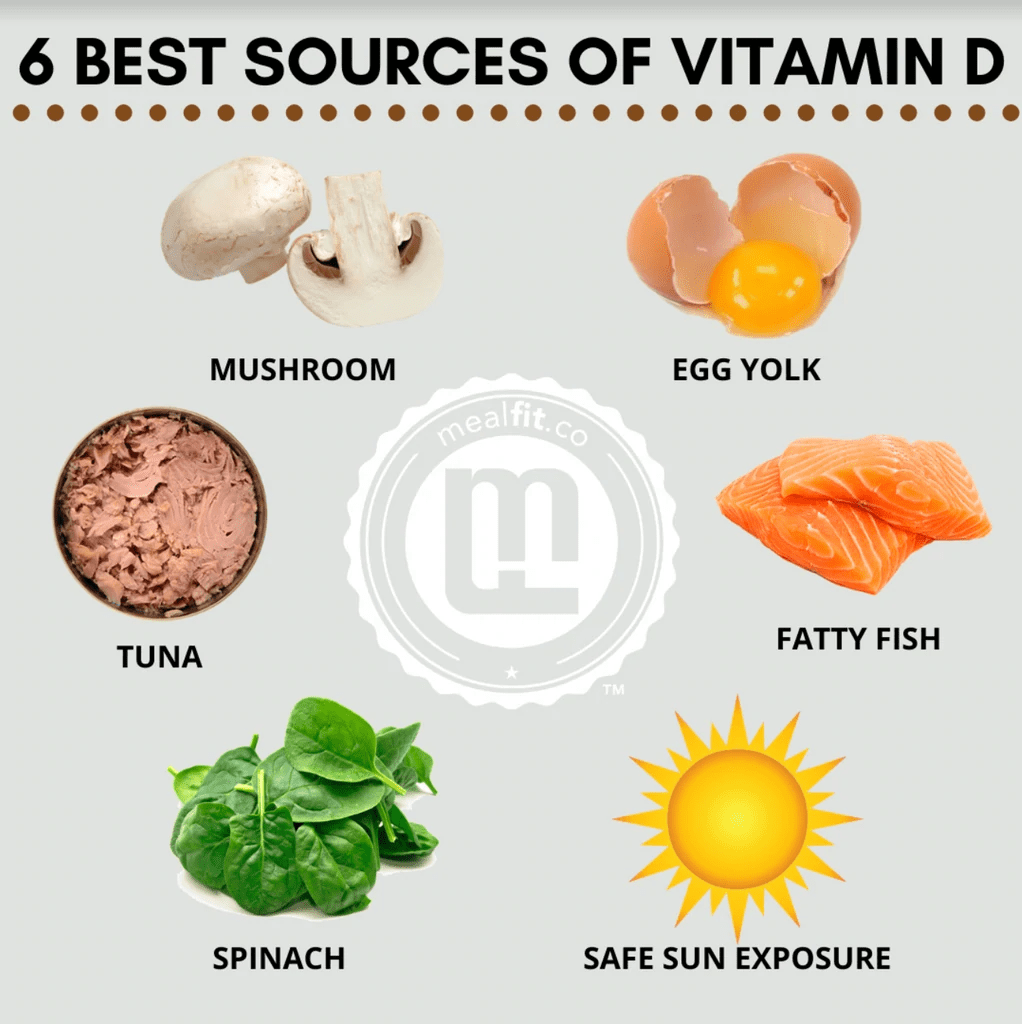
Vitamin D is derived naturally from two sources: the sun and food (Cannell & Hollis, 2008). Certain foods are especially high in vitamin D, namely wild fatty fish, shitake mushrooms, and wild meats (i.e., reindeer) while some processed foods are fortified with said vitamin (i.e., breakfast cereals, milk) (Cannell & Hollis, 2008). Vitamin D production comes primarily from the sun (in regions with abundant sun exposure); when UVB light contacts the skin, it converts cholesterol in the blood (7-dehydro-cholesterol) into vitamin D3 (Cannell & Hollis, 2008). Modest amounts of sun exposure can produce concentrations of D3 that exceeds levels found in food; 30 minutes of sun exposure on a fair skinned individual produces the equivalent of 200 glasses of vitamin D3 found in milk (Cannell & Hollis, 2008). However, individuals living in northern climates (i.e., 125 million people) receive little sun exposure, demanding another alternative; vitamin D supplementation (Chaplin & Jablonski, 2013)
SUPPLEMENTS

As mentioned in the last section, vitamin D3 can be supplemented if individuals do not have access to wild caught fatty fish, or if they live in regions with infrequent sun exposure. Due to the aforementioned influences of vitamin D3 upon genes and organs in the body, supplementation has become a viable, and necessary, alternative. Vitamin D3 is often available in 1000 international units (IU) and as high as 50,000 IU in pill form (Cannell & Hollis, 2008). Once digested and absorbed into the bloodstream, supplemental D3 is converted into calcidiol, also known as (25(OH)D) (Cannell & Hollis, 2008). Despite the origin of D3 (sunlight, fatty fish, supplementation) all forms of vitamin D convert into (25(OH)D) in the bloodstream by the liver, eventually converting into its active form; 1,25(OH)D, which directly interfaces with VDRs (Cannell & Hollis, 2008). Having considered the utility, sources, and forms of vitamin D3, the following will explore methods of measuring said vitamin. Since evidence indicates a wide physiological reach and influence of vitamin D, in addition to difficulty for certain populations to acquire adequate vitamin D, measuring and tracking said micronutrient is critical. However, it is also pertinent to measure the correct form of vitamin D via blood analysis.
MEASURING VITAMIN D
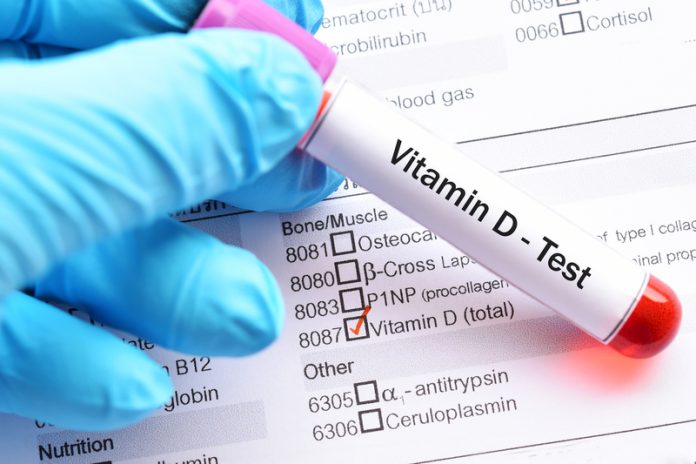
Although1,25(OH)D is the biochemically active form of vitamin D, said micronutrient tells little about the overall storage and availability within the human body; 1,25(OH)D only indicates that the kidney is creating and managing its concentrations (Cannell & Hollis, 2008). Such a scenario might be mildly analogous to a fuel gauge in a car; the gauge could measure gasoline levels and concentrations as they entered the engine, but would not be very telling of how much fuel is left in the tank. The second method of measurement is more relevant and useful as it allows one to avoid having the engine stall from low fuel levels. The second measurement also allows one to monitor and pre-emptively plan for refueling.Measuring and monitoring (25(OH)D) serves a similar purpose, allowing nutritionists and medical professionals to know if vitamin D levels are adequate enough to avoid deficiencies. Although it is paramount to avoid low levels of (25(OH)D), evidence suggests that optimization of said micronutrient is key to maintaining overall health and longevity (Cannell & Hollis, 2008).
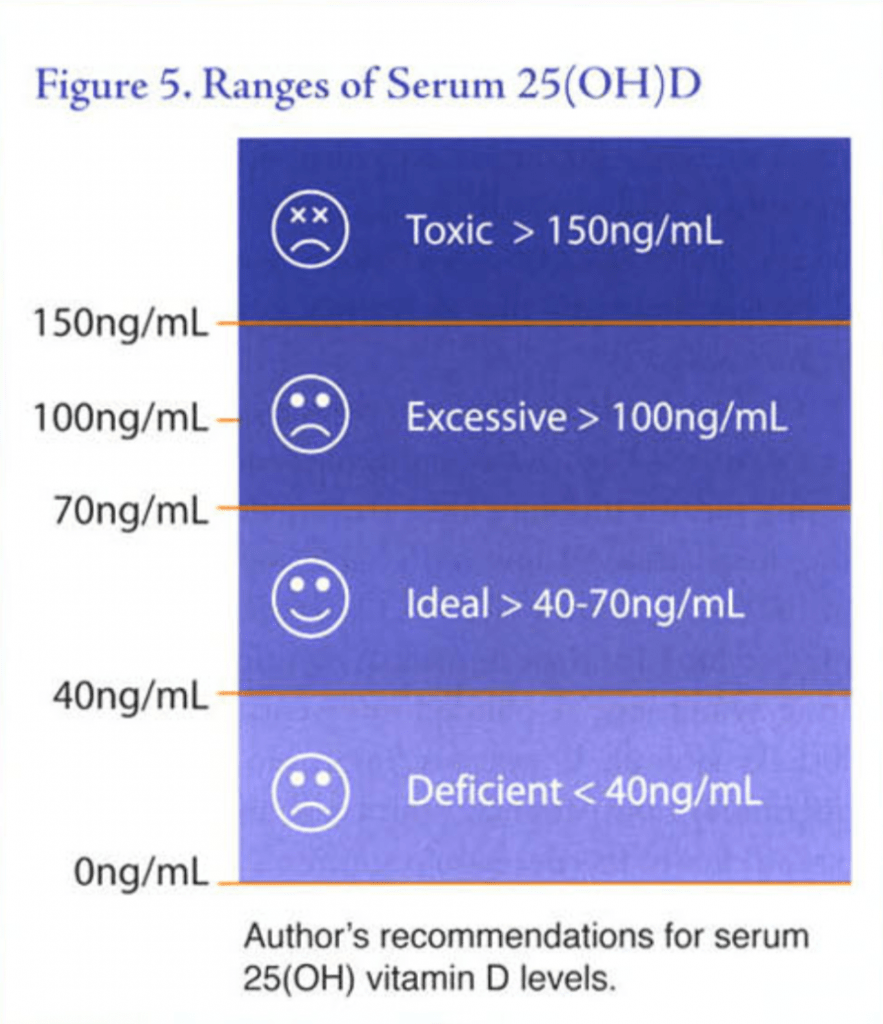
OPTIMAL VITAMIN D LEVELS

Individuals living in sun-rich environments tend to have (25(OH)D) levels between 50-70 ng/ml. Yet vitamin D insufficiency (<20ng/ml), according to Rosen (2011), is as high as the high as 50% to 80% in North America due to a lack of adequate sun exposure and foods rich in vitamin D3. Cannell and Hollis (2008) provided a chart (see below) that helps professionals and patients identify (25(OH)D) levels along a spectrum. Deficiency can be defined as (25(OH)D) levels below 40 ng/ml, while 70–150 ng/ml is excessive, and >150 ng/ml is considered toxic. The optimal level of (25(OH)D) is considered between 40-70 ng/ml (Cannell & Hollis, 2008). Although awareness of optimal levels helps direct individuals to proper supplementation, recommended dosages of vitamin D are influenced by multiple factors such as body weight, body fat, age, presence of inflammatory bowel disease, gluten enteropathy, gastric surgery, biliary disease, or intestinal overgrowth, use of anti-seizure medications and long-term use of glucocorticoids (Cannell & Hollis, 2008; Rosen, 2011). As such, Cannell and Hollis (2008) recommended consuming 1000 IU of vitamin D3 for every 15 kg of bodyweight. Such an approach serves as a starting point, in conjunction with routinely measuring (25(OH)D) levels.
VITAMIN D RANGES
In conclusion, vitamin D3 plays a key role in overall health and longevity as it interacts with, and influences, over 200 genes and multiple organs within the human body. If sun exposure is poor/unavailable and there is a lack of access to fatty fish sources, supplementation of vitamin D3 is a viable option for such a population. As an aggregate, supplementation of vitamin D3 and periodic monitoring of (25(OH)D) levels should help individuals achieve optimal health and a better quality of life.
References
Cannell, J. J., & Hollis, B. W. (2008). Use of vitamin D in clinical practice. Alternative Medicine Review, 13(1), 6-20.
Chaplin, G., & Jablonski, N. G. (2013). The human environment and the vitamin D compromise; Scotland as a case study in human biocultural adaptation and disease in susceptibility. Human Biology, 85(4), 529-552.
Rosen, C. J. (2011). Vitamin D Insufficiency. The New England Journal of Medicine, 364(3), 248-254.
Wang, Y., Zhu, J., & DeLuca, H. F. (2012). Where is the vitamin D receptor? Archives of Biochemistry and Biophysics, 523(1), 123-133.
-Michael McIsaac
