Vitamin D3 has been widely recognized as a key player in controlling metabolic bone disease. Less known to the public is said vitamin’s role in anti-inflammatory and immune-modulating capabilities (Raman, Milestone, Walters, Hart, & Ghosh, 2011). Interestingly, many tissues and cells, to include the immune system, contain vitamin D receptors (VDRs), indicating a need for its presence (Raman et al., 2011).
Irritable bowel disease (IBD), including ulcerative colitis (UC) and Crohn’s disease (CD), are postulated to manifest from a complex interaction of genetic, environmental, and microbial factors (Raman et al., 2011). Furthermore, Raman et al. (2011) suggested that CD and UC are thought to engage in an aberrant activation of the mucosal immune system. Specifically, there is an over-production of pro-inflammatory cytokines (proteins that signal inflammatory immune responses from other cells) including interferon-γ (IFN- γ) and tumor necrosis factor-alpha (TNF-α) (Raman et al., 2011). Said cytokines come from a dysregulated T-cell (white blood cell involved in cell-mediated immunity) activity to include CD4+ (glycoprotein on T-helper cells) and type-1 lymphocytes (Raman et al., 2011).
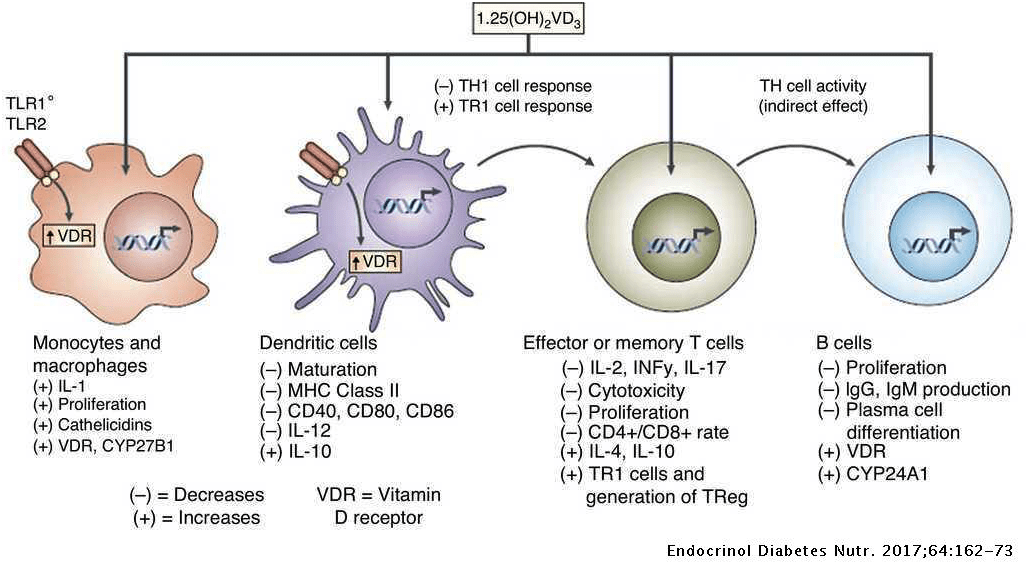
Of particular interest is that VDRs are found on monocytes (white blood cells), as well as leucocytes and CD4+ (Raman et al., 2011). Furthermore, Raman et al. (2011) indicated that dendritic cells (antigen-presenting cells) and T lymphocytes (white blood cell) both synthesize 1,25 (OH)2D3 suggesting a need and relationship to vitamin D3and immune system regulation. Furthermore, Raman et al. (2011) stated that there is abundant evidence demonstrating that 1,25 (OH)2D3 directly down regulates T-cell (involved in cell mediated immunity) activity and propagation, ultimately taming the cell-mediated immune response.
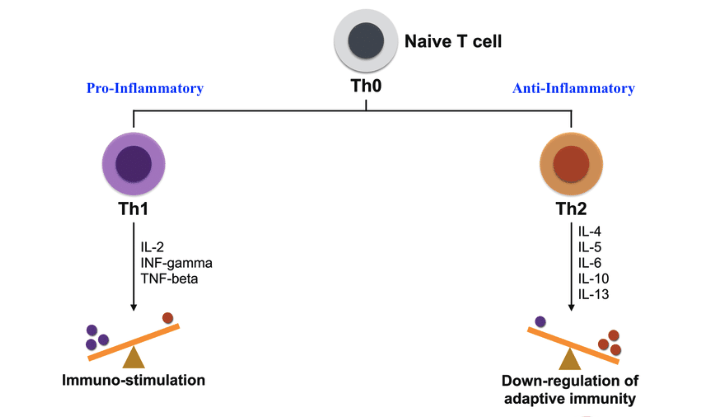
Interleukin (IL-12), produced by DCs/macrophages/neutrophils, is a cytokine that induces pro-inflammatory processes like Th1 (a T helper cell that mounts an immune response within a cell) specialization, which is involved in the development of IBD (Raman et al., 2011). 1,25 (OH)2D3 helps inhibit IL-12 production while stimulating IL-10 (an anti-inflammatory cytokine) that produces Th2 (a T helper cell that mounts an immune response outside of cells). Furthermore, IL-10 also inhibits other pro-inflammatory monokines (produced by macrophages and monocytes) such as IL-6, IL-1, and TNF-α (Raman et al., 2011).
In conclusion, VDRs and vitamin D3 shares an intimate relationship with many cells and tissues in the body, to include the immune system. Said vitamin has been implicated in the down-regulation of inflammatory processes associated with IBD, while promoting anti-inflammatory responses. As such, it is possible that vitamin D3 supplementation (or via sunlight exposure) can help control the extent to which IBS can manifest.
References
Raman, M., Milestone, A. N., Walters, J. R. F., Hart, A. L., & Ghosh, S. (2011). Vitamin D and gastrointestinal diseases: Inflammatory bowel disease and colorectal cancer. Therapeutic Advances in Gastroenterology, 4(1), 49-62.
-Michael McIsaac
