Vitamin D3 (VD) is largely known as a key nutrient in controlling metabolic bone disease. However, VD’s role in immune-modulating and anti-inflammatory capabilities has become increasingly recognized.1Interestingly, many tissues and cells, to include the immune system, contain vitamin D receptors (VDRs), indicating an intimate relationship between said nutrient and cell function.1(49) However, large portions of humans (i.e., 2% or 125 million people) live in latitudes which deny exposure to the sun; a primary medium in which VD is derived.2 As such, deficiencies in VD are common, and associated with disease states such as prostate cancer (PC). As a means of appreciating VD and its relationship to PC, the following will explore the same.

In this author’s previous posts, dietary interventions and their relationship to health (i.e., reducing cancer rates) were considered. However, as stated above, VD is procured primarily from sunlight exposure; an option limited in northern latitudes. Although such diets like the Mediterranean diet (MD) and ketogenic diet (KD) have demonstrated favorable effects on health markers, both interventions can potentially lack adequate amounts of VD if individuals are not consuming such foods as fatty fish, shitake mushrooms, and wild meats on a regular basis.3 Since individuals who live in sun-rich environments tend to have levels of VD (measured as 25-hydroxyvitamin D, or 25OHD, in the blood) between 50-70 ng/ml, it is highly probable individuals in low sun exposure environments are not receiving and producing optimal levels of 25OHD.4
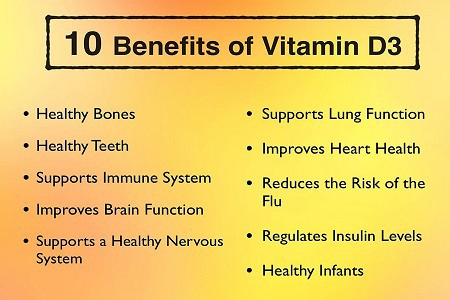
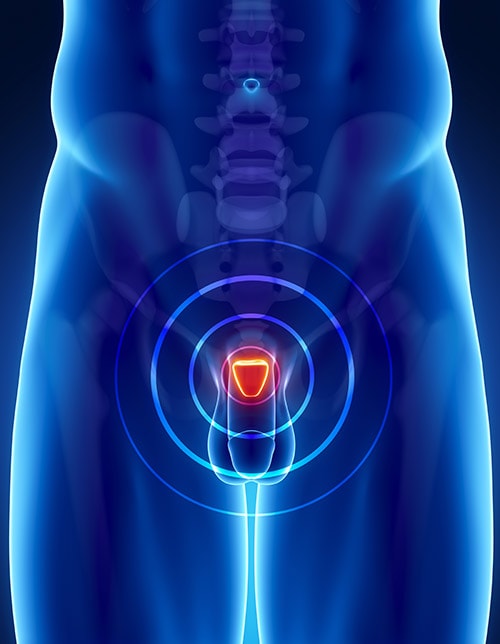
Since VD interacts with more than 200 genes in the body and tissues/organs (i.e., intestinal epithelium, renal tubules, parathyroid gland cells, skin, mammary epithelium, pancreas, pituitary gland, skeleton, immune system, and germ tissues), having optimal 25OHD levels is paramount.5 Furthermore, diseases such as PC have strong associations with low 25OHD levels in the blood, with a high probability of concomitant deficiencies in the aforementioned tissues and organs, likely inducing other unfavorable systemic effects while cancer continues to manifest. PC is the most common malignancy among men, worldwide, and thus demands close focus and intervention if said disease is to be managed and prevented in a meaningful and efficacious fashion.6 As such, the following sections will consider epidemiological studies from Sahin et al6 linking the risk and outcome of vitamin D with PC in greater detail.
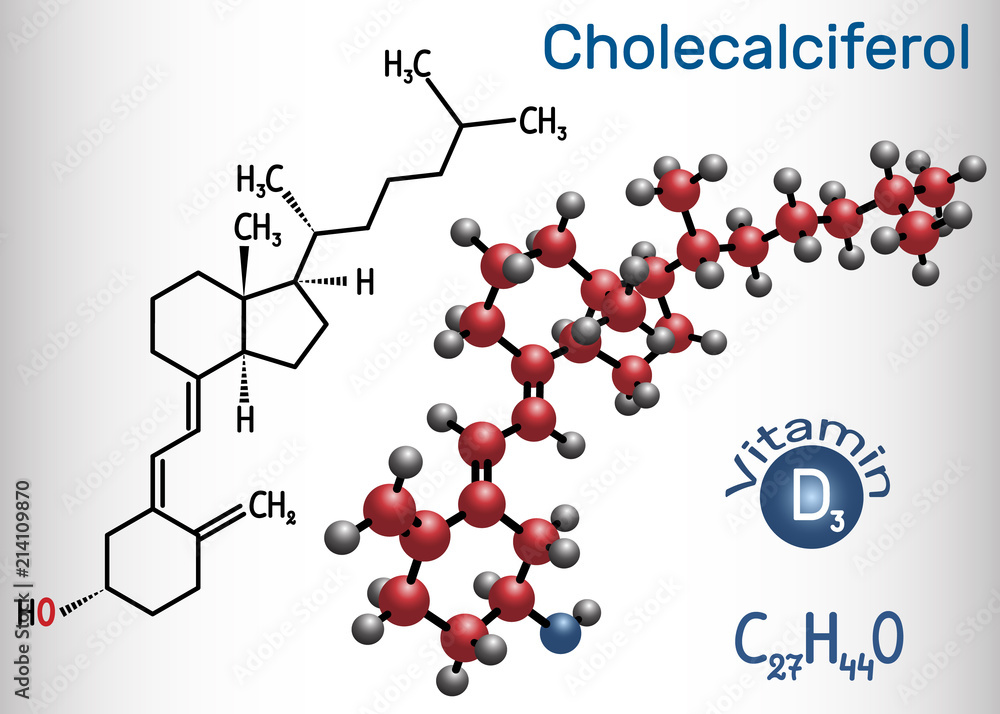
A case control study (observational study comparing two groups and respective outcomes) was conducted by Sahin et al6(113) whereby individuals diagnosed with PC and benign prostatic hyperplasia (benign prostate enlargement, also known as BPH) who were admitted into the researchers’ urology clinic between 2017 and 2019 were included in the study. Furthermore, all cases were newly diagnosed, followed up and confirmed with PC and BPH with histopathological methods. However, patients with metastatic PC, or who underwent hormonal therapy, and/or who experienced recent severe weight loss were excluded from the study.6(113) Finally, the study was conducted with a total of 256 patients aged (47 to 86 years of age) between 2018 and 2019. The mean age of 128 patients with PC was 67.70±7.74 years, and the mean age of 128 patients with BPH was 67.03±7.89 years.6(114) Serum 25OHD and 1,25-dihydroxyvitamin D (the biologically active form of VD, also known as 1,25DOHD) levels were measured to assess vitamin D status.6(114)
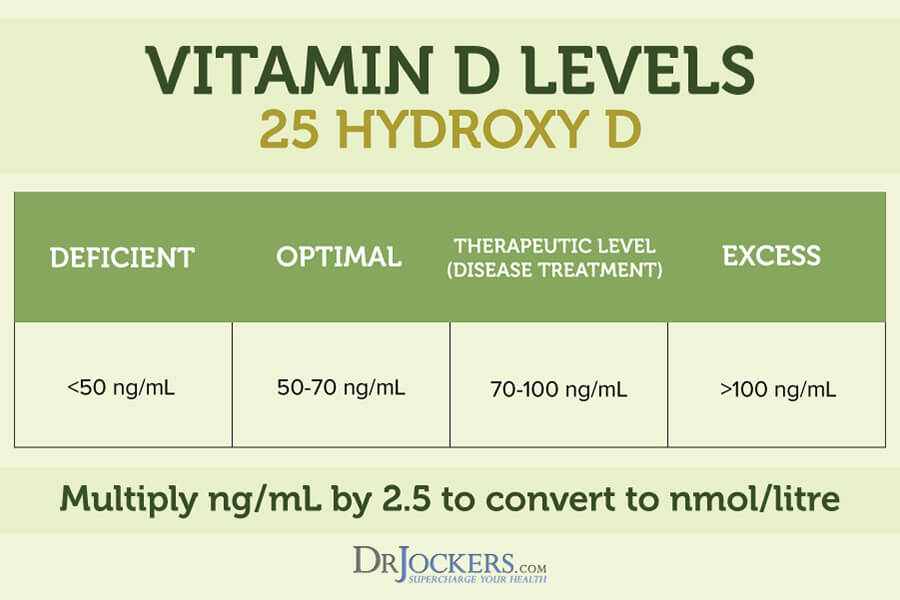
Sahin et al6(114) stated that low levels of 25OHD (<20 ng/ml) is considered inadequate. Furthermore, when VD intake is optimal, evidence has supported a distinct dysfunction/ inhibition of PC cell proliferation, cell invasion, anti-angiogenesis (production of new blood vessels), decreased cell differentiation, increased apoptosis, and altered gene expression. Of particular interest found from the observational study of Sahin et al1(114) was a statistically significant difference between the 25OHD levels of BPH and PC patients; individuals with BPH had higher levels of 25OHD that PC groups. Such a result suggests that the progression from benign tumors to those of a malignant form, has an inverse relationship to 25OHD. Considering the known influence of optimal 25OHD levels upon cancer cell growth and proliferation, such knowledge might be useful for individuals found to have early stages of BPH; if said individuals have lower levels of 25OHD, increasing VD intake might be indicated as a preventative measure.
In conclusion, PC is the most common malignancy among men, worldwide, and thus demands close focus and intervention if said disease is to be managed and prevented in a meaningful and efficacious fashion. In addition to a diet rich in healthy fats, fiber, protein, and phytonutrients, supplemental VD is likely to be a necessary adjunct, especially amongst individuals with low sun exposure.
References
1. Raman M, Milestone AN, Walters, JRF, Hart AL, et al. Vitamin D and gastrointestinal diseases: Inflammatory bowel disease and colorectal cancer. Therap Adv Gastroenterol. 2011;4(1):49-62. doi:10.1177/1756283X10377820.
2. Chaplin G, Jablonski NG. The human environment and the vitamin D compromise; Scotland as a case study in human biocultural adaptation and disease in susceptibility. Hum Bio. 2013; 85(4):529-552. doi:10.3378/027.085.0402.
3. Cannell JJ, Hollis, BW. Use of vitamin D in clinical practice. Altern Med Rev. 2008;13(1):6-20. Retrieved from http://archive.foundationalmedicinereview.com/publications/13/1/6.pdf
4. Rosen CJ. Vitamin D Insufficiency. N Engl J Med. 2011;364(3):248-254. doi: 10.1056/NEJMcp1009570.
5. Wang Y, Zhu J, DeLuca HF. Where is the vitamin D receptor? Arch Biochem Biophys. 2012;523(1):123-133.doi:doi:10.1016/j.abb.2012.04.001.
6. Sahin A, Toprak T, Kutluhan MA, et al. Is prostate cancer related to low vitamin D level? DOAJ. 2019;18:113-116. Doi:10.4274/uob.galenos.2019.1221.
-Michael McIsaac
