
Diabetes mellitus is both a progressive and chronic disease in which there exists an inability to effectively and efficiently metabolize fats, proteins, and carbohydrates. Ultimately, such a condition leads to hyperglycemia, or elevated blood glucose levels, and eventually type 2 diabetes (T2D). Several posts have been written by this author regarding sleep/nutritional/supplemental interventions and their effects upon insulin resistance/T2D. However, it is critical that one is reminded of the role physical activity plays in the management and prevention of T2D, as part of a larger and more inclusive approach. As such, the following will explore the same.
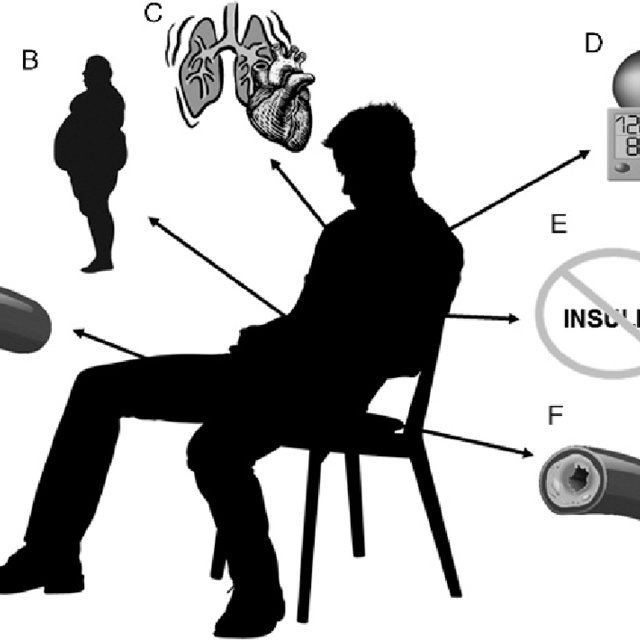
Physical inactivity and sedentary behavior are relatively prevalent phenomenons, in addition to poor nutrition, and is estimated to occur amongst 57% of Canadians.2 Furthermore, such lifestyle choices also contribute to insulin resistance and T2D, demanding change and intervention. Structured physical activity, which can include resistance training and aerobic exercise, have been associated with long-term control of blood glucose, measured as hemoglobin A1C (HBA1C).1(220) Such outcomes are produced from approximately 150 minutes of physical activity per week.1(220)
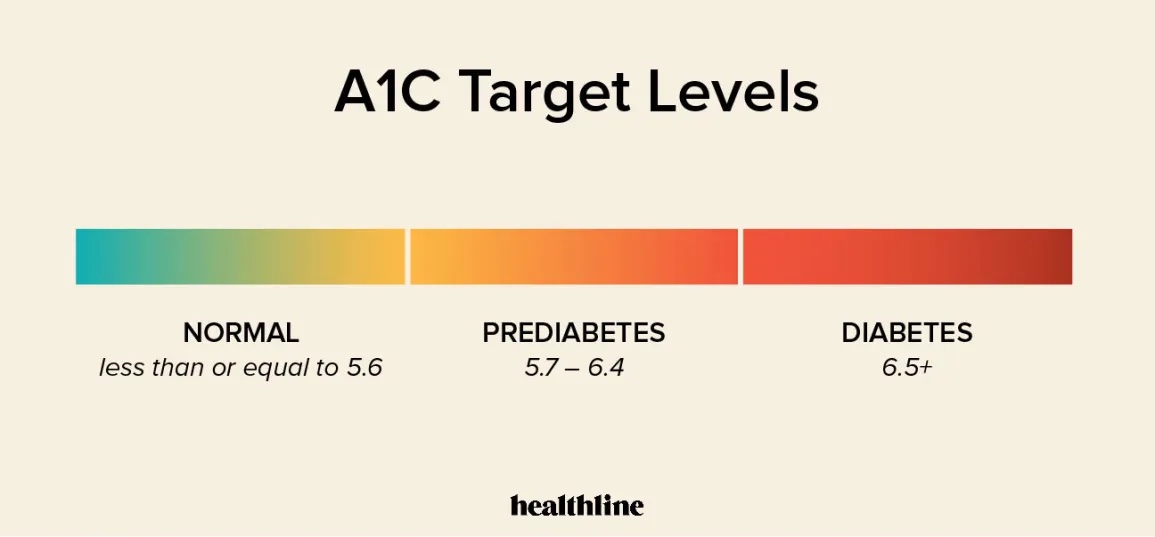
HBA1C is a pertinent biomarker, and worthy of controlling, because it elucidates and tracks the influence of T2D over weeks and months. Due to the short-term and long-term complications of T2D (i.e., blindness, kidney disease, nerve degradation, vascular disorders, stroke, heart attack), it behooves exercise professionals and nutritionists to provide at-risk individuals opportunities and avenues to circumvent and/or manage such conditions.1(220) Physical activity, as stated by Asprina et al,1(220) is an essential pillar for managing T2D, in addition to nutritional and pharmacological interventions.

Asprina et al1(221) stated that 150 minutes per week of physical activity can be further broken down into 3 resistance training sessions per week with moderate aerobic exercise. Such a combination has been shown to support improvements not only in blood glucose regulation, but also blood lipid profiles, blood pressure, and the ability to conduct work with less fatigue.1(221) Furthermore, physical inactivity is suggested to account as a principal cause for 21-25% of breast/colon cancer, 30% ischemic heart disease, and 27% of diabetes mellitus.1(221) Despite the potential complications of inactivity, interventions can be simple, yet effective, to include walking.
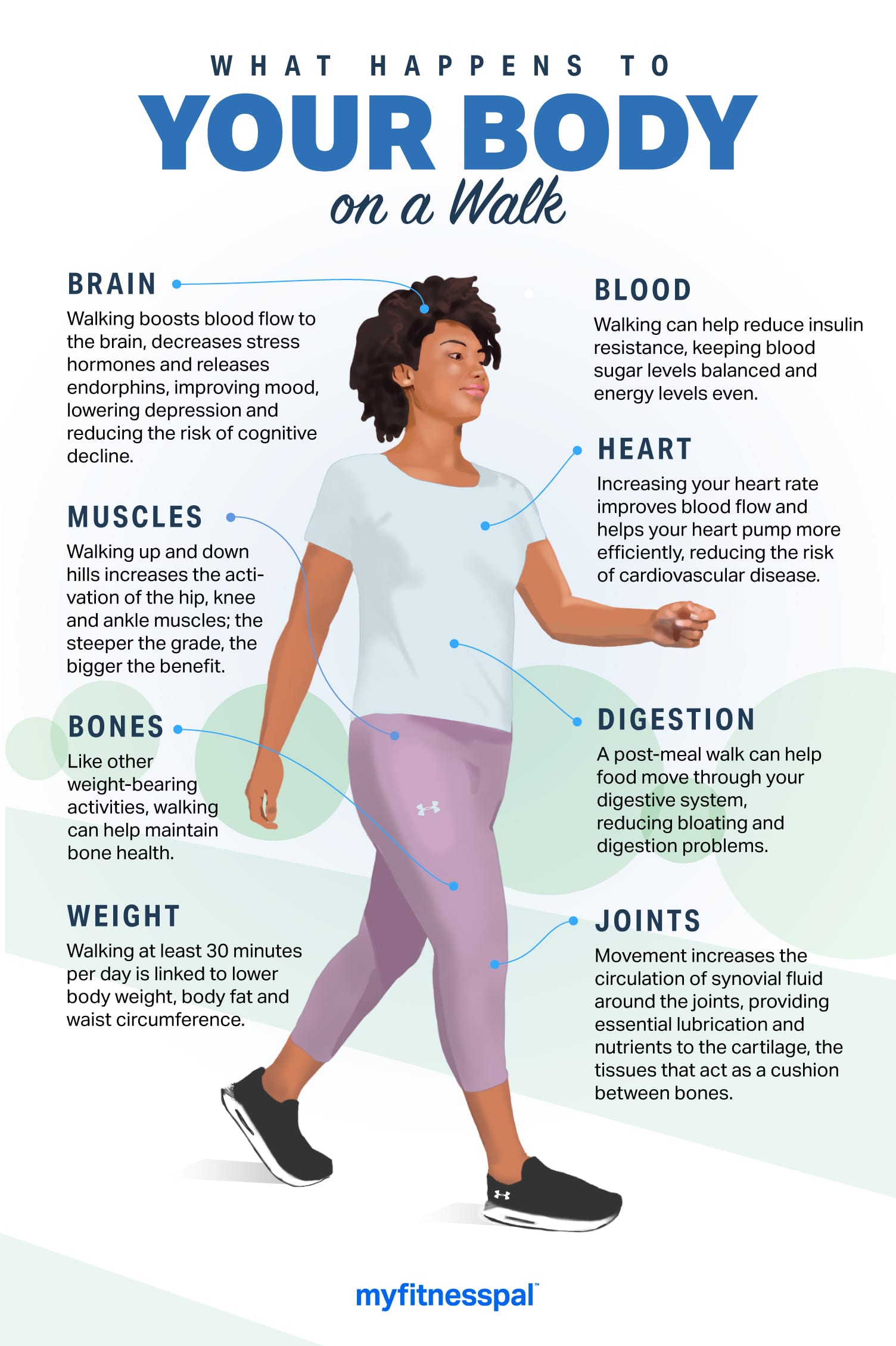
Walking is a form of activity that is simple, safe, cost effective, and physiologically beneficial. Furthermore, walking helps improve muscular/cardiovascular endurance, mobility, reduces hypertension, heart disease, probability of stroke, and weight loss.1(222) Walking is beneficial for glucose control due to its influence upon glucose transporters (GLUT4) found on cell membranes. Walking (a pattern of muscle contractions) induces migration of GLUT4, a transporter protein, to the cell surface. Such a process is paramount as GLUT4 pulls glucose out of the blood and into the cells, via facilitated diffusion, for ATP (energy) production.1(222) Ultimately, said process controls hyperglycemia and downstream effects thereof.
In conclusion, diabetes mellitus is both a progressive and chronic disease in which there exists an inability to effectively and efficiently metabolize fats, proteins, and carbohydrates. Ultimately, such a condition leads to hyperglycemia, or elevated blood glucose levels, and eventually T2D. Evidence suggests that in conjunction to nutrition and pharmacological interventions, movement in the form of moderate aerobic exercise, has been shown to support favorable changes in HBA1C, in addition to other relevant biomarkers. Such simple, safe, and cost-effective interventions should help incentivize individuals with insulin resistance/T2D to implement the same.
References
1. Asprina, Taufiq I, Rajiani I. Walking as an alternative treatment for HBA1C levels control among type 2 diabetes mellitus patients. Indian J Public Health Res Dev. 2018;9(9):220-223. doi:10.5958/0976-5506.2018.00998.
2. Meckling KA, Sherfey, R. A randomized trial of a hypocaloric high-protein diet, with and without exercise, on weight loss, fitness, and markers of the metabolic syndrome in overweight and obese women. Appl Physiol Nutr Metab. 2007;32(4):743-752. doi:10.1139/H07-059.
-Michael McIsaac
