
Childhood obesity is considered the greatest public health challenge to date, according to Zinn et al.1 Furthermore, obesity in said age group has increased to more than double over a 30-year period, worldwide, and continues to escalate.1(1) Such unsettling truths have placed children at a higher risk of developing metabolic disorders as adults, behooving nutritionists and researchers to develop strategies that can prevent and manage the epidemic. The following will consider a whole-foods/restricted carbohydrate approach in managing such a growing global problem.
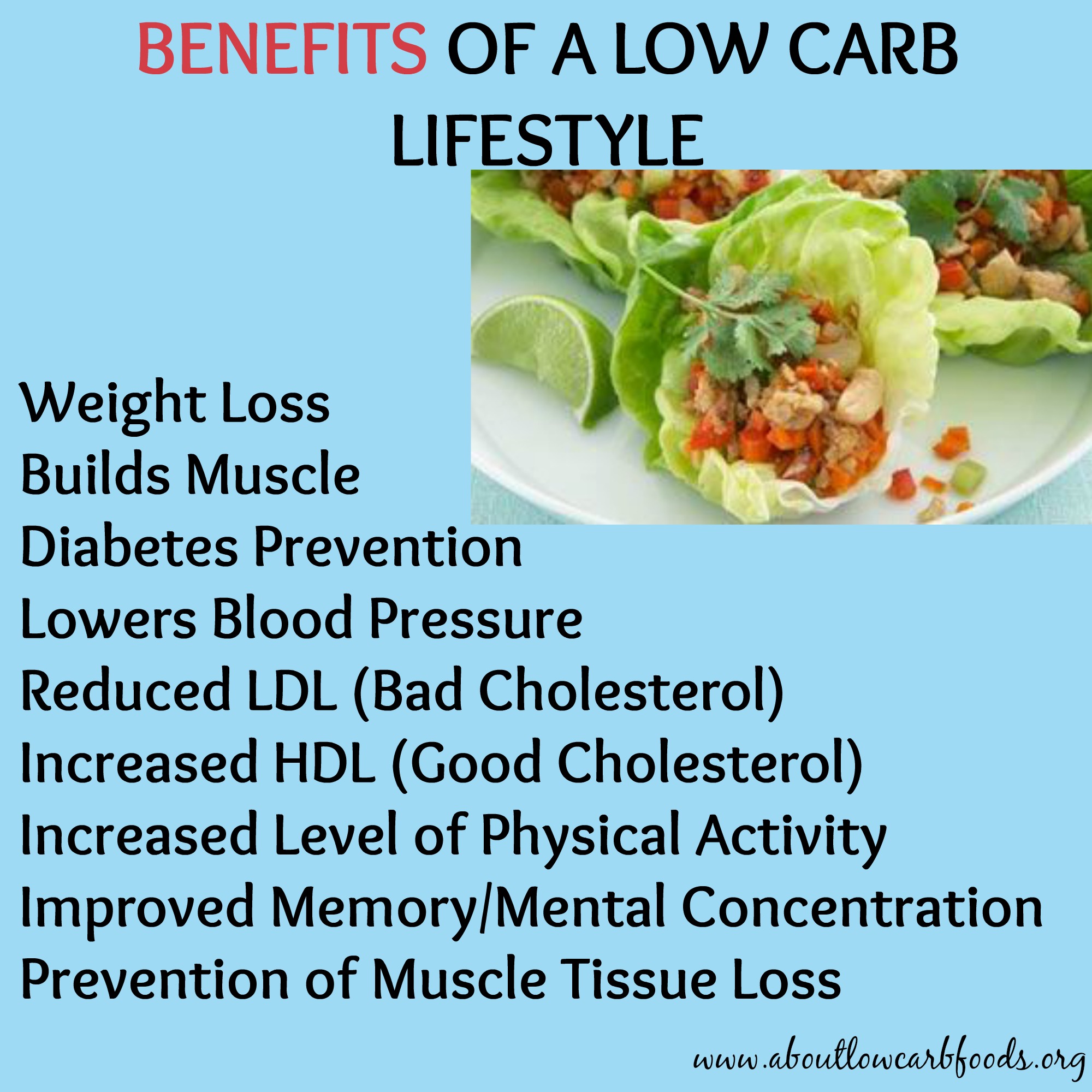
Although dietary recommendations and interventions have been implemented to slow the progression of childhood obesity, the number of children who are obese has continued to grow and expand its reach.1(1) Approximately 50 years ago, dietary guidelines recommended a moderate-to-high carbohydrate intake with moderate protein and low-fat intake.1(1)Recent research in carbohydrate-restricted and higher fat dietary approaches have emerged and grown in popularity for both children and adults in managing weight and metabolic disorders. Research has suggested such approaches are at least as effective as other nutritional interventions with the added benefit of lowering triglycerides, increasing high density lipoprotein (HDL) cholesterol, and improving glycemic control.1(1) As such, the following will explore the feasibility of a high fat, low carbohydrate (HFLC) approach.

Zinn et al.1(2) stated that although HFLC foods are effective in treating obese/metabolically deranged individuals, such dietary approaches have been criticized as lacking data around adherence and affordability; constituents that can dissolve long-term habitual changes. As a means of identifying the feasibility of HFLC diets, the researchers recruited 25 obese children in New Zealand (8-13 years of age) who underwent a 12-week whole food HFLC intervention.1(2)Participants, including caregivers, were invited to a 90-minute workshop in which an endocrinologist and dietician explained the entire experiment and nutritional guidelines. The following will cover the same in greater detail.
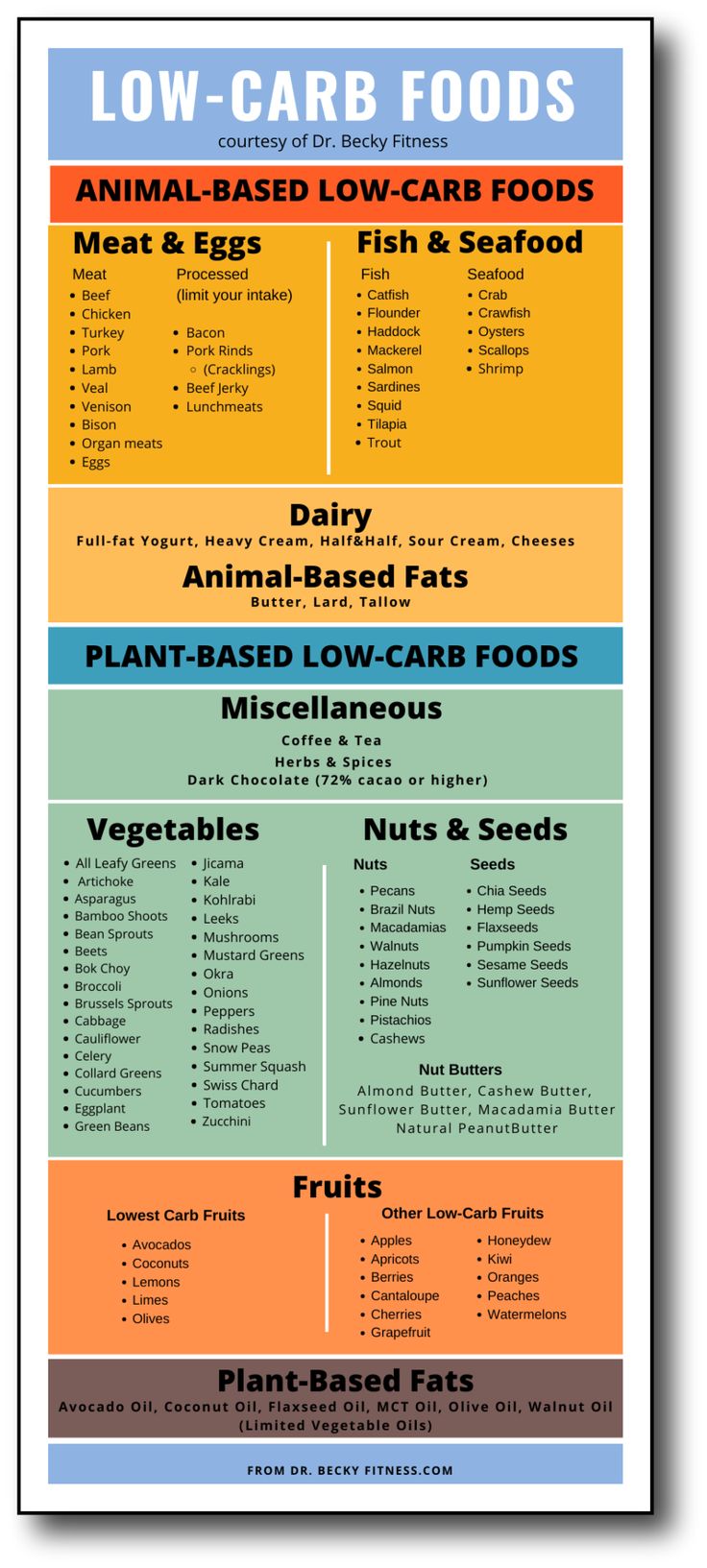
The endocrinologist and dietician explained that the main goal of the experiment was to minimize/discourage processed food consumption when and where possible and to encourage whole foods instead. Furthermore, participants were not provided with a strict and/or individualized nutrition plan or particulars behind macronutrient breakdowns.1(2) Rather, participants were provided with a food guide upon which they could choose foods from two major categories: preferred foods and foods to avoid.1(2) The goal was to have participants consume less than the minimum carbohydrate guidelines set forth in the New Zealand food and nutrition guidelines.
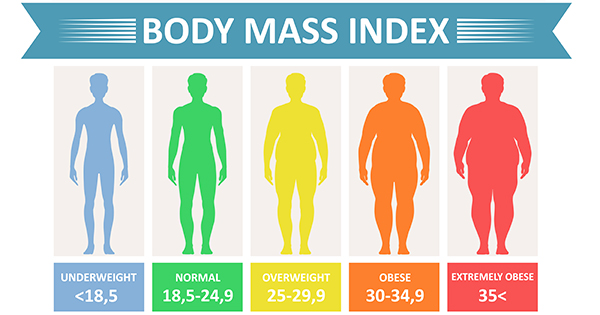
Preferred foods included non-starchy vegetables, fruit, eggs, meat, full dairy, nuts, seeds, avocado, avocado oil, and olive oil. Foods that were discouraged included packaged foods, grains, cereals, and foods with refined sugar.2(2)Outcome variables measured for the experiment included acceptability, adherence, and affordability which were ascertained by weekly telephone conversations with caregivers and focus groups at the end of the 12 week experiment.1(2) Other measures considered were changes in BMI, weight, fasting HDL/total cholesterol/low density lipoproteins (LDLs), serum glucose, hemoglobin A1C, and serum insulin.1(2)

Of the 25 children enrolled in the 12-week HFLC experiment, 13 completed the program. Results indicated that the majority of the parents and children found the food choices to be acceptable, generally consuming more eggs, cheese, nuts, and fruit than before the intervention.1(4) Adherence, interestingly, was directly related to family support; if caregivers encouraged children to follow the guidelines adherence was high. When there was little support, adherence fell.1(5) Reports of affordability were mixed; caregivers supported LCHF if usual foods were not being purchased, but showed discontent if new foods were purchased in addition to conventional foods.1(6)Finally, biomarker measurements were markedly improved compared to baseline; significant weight loss was noted in addition to a significant increase in HDLs and triglyceride to HDL ratios. Such improved ratios are useful predictors of insulin resistance, which is a constituent in metabolic syndrome.1(6)

In conclusion, the study by Zinn et al.1(6) suggested that the LCHF diet appears feasible. However, limitations within the study included a low sample size and a relatively short experimental period (i.e., 12 weeks). Despite the low sample size and brief experimental period, such data should encourage researchers to develop and conduct larger, more robust, experiments addressing said limitations. Most importantly, the LCHF approach can provide parents and children a possible, and safer, alternative to processed food consumption.
References
1. Zinn C, Schmiedel O, McPhee J, Harris N, et al. A 12-week whole-food carbohydrate-restricted feasibility study in overweight children. Journal of Insulin Resistance.2018;3(1):e1-e9. doi:10.4102/jir.v3i1.42.
-Michael McIsaac
