Kinesiology is an emerging field, slowly finding its place amongst other allied health and health care professions. Historically, Kinesiology is new, compared to the inception and growth of other established professions (i.e., massage therapy, physiotherapy, chiropractic, and medicine). Often, (I do not believe this to be intentional), our message, scope of practice, and efficaciousness appears underappreciated and misinterpreted, especially as it relates to post-rehabilitation.
In the following sections, I would like to explore the intricate nature of our work, using evidence-based approaches and research, as a means of revealing why we require time with clients to affect meaningful changes in their strength, and quality of life. It is my hope that the following information will liberate individuals from misconceptions and assumptions they may have about my field, scope of practice, intentions, and approaches.

Post-rehabilitation (PR) clients require meticulous and thoroughly developed training programs. Extensive weakness and deconditioning are common traits among the aforementioned populace, and risk of re-injury is high. PR clients are often seeing a medical professional, or have been recently discharged. Their injuries are usually resolved/controlled, but they are often not ready to withstand the rigors of daily activity and work related tasks. Such a situation requires program design and training approaches deeply imbedded in pragmatic and sound evidence-based methods.
Skill acquisition (i.e., improving poor postures, faulty movement patterns, and performing exercises appropriately) requires time, problem solving, and refinement (Magill, 2011). In the case of a PR client, the aforementioned process must be accompanied by a method that reduces the exposure to undesirable movement patterns and habits, which may exacerbate injured regions (Page, Lardner, & Frank, 2010). Most PR clients have little-to-no prior exercise experience, making this requirement exceedingly pertinent in my practice. Movements must be gentle, concise, purposeful, and yet progressive in nature to yield improvements in mobility, stability, and full body strength over time.
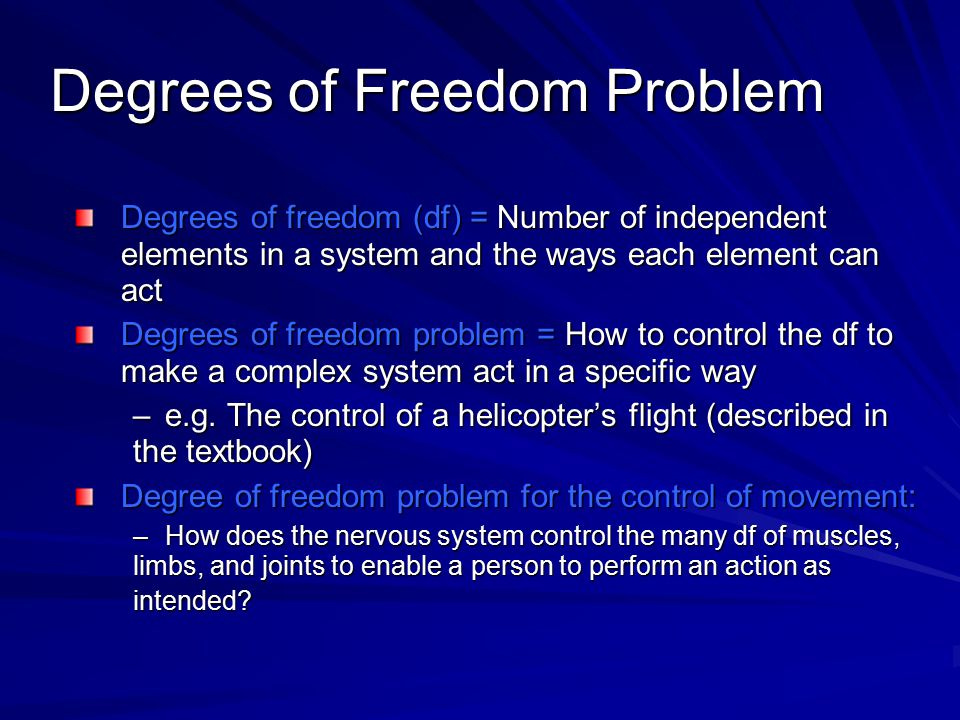
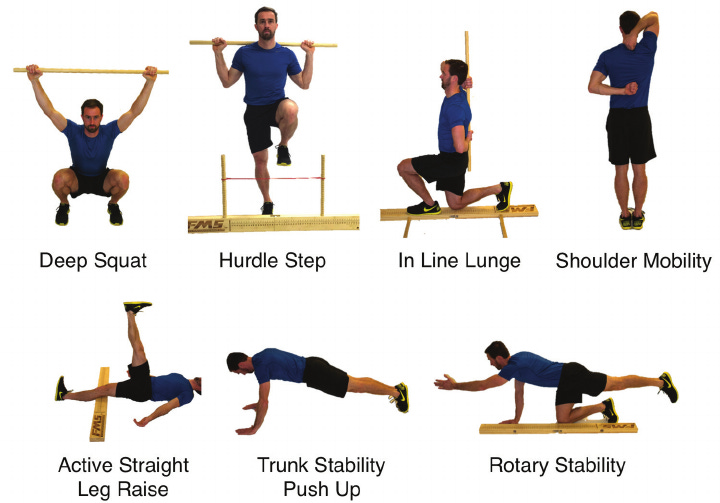
Injured clients must learn and acquire fundamental movements that are used in work and daily activity such as squatting, lifting, pushing, pulling, carrying, and locomotion. Despite the nature of injury, all individuals must reintegrate their injured regions back into the aforementioned functional motions. However, complex exercise involves controlling the joints of the body in a coordinated and harmonious fashion. Magill (2011) referred to this as the degrees of freedom problem.
Often, novices will become “stiff” and lock out many joints when they are initially exposed to novel exercises, often leading to undesirable muscle spasms and inefficient movement. Furthermore, PR clientele often have trigger points, which inhibit smooth and coordinated force production along local/global muscles, joints, and ultimately, exercise (Bron, Dommerholt, Stegenga, Wensing, & Oostendorp, 2011). Additionally, poor movement can further exacerbate the originally injured region.
In essence, a vicious cycle begins, which feeds pain and deeper movement dysfunction, commonly known as the chronic musculoskeletal pain cycle (Page et al., 2010). Thus, post-rehabilitation requires a multifaceted and dynamic approach, which addresses all “roadblocks” derived from the initial injury, before strengthening the client in a meaningful and effective fashion.
Physical function may be thought of as goal-directed movement, considered the link between physical actions, colloquially defined as movement, and the environment in which it takes place (Cech & Martin, 2012). Such characteristics are essential, as they permit individuals to survive, adapt, and learn within the environment (Cech & Martin, 2012). If movement is inhibited or dysfunctional (i.e., as seen in PR clients), an individual may be less able to participate in goal directed movement, in a safe and efficient manner.
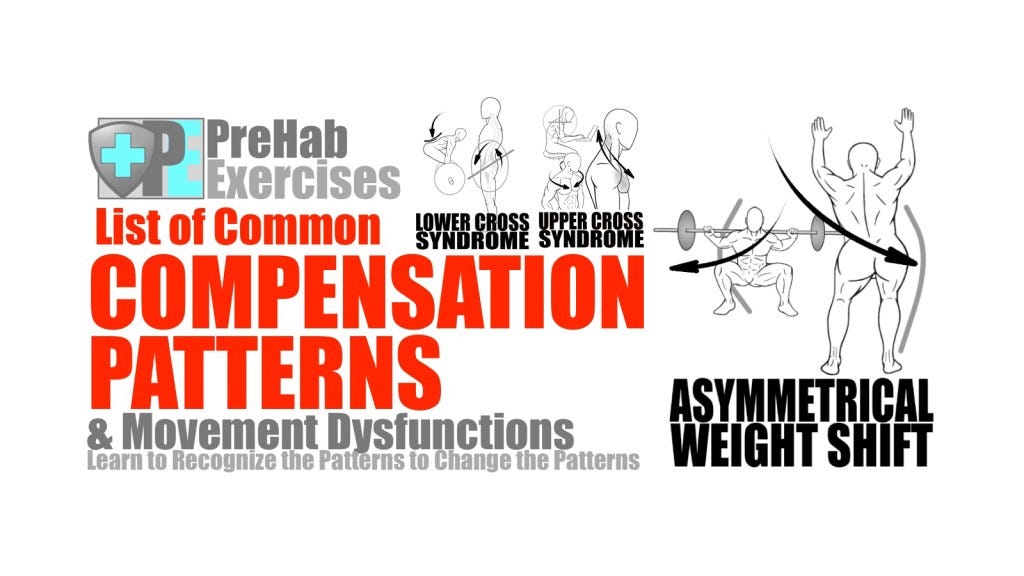
Movement dysfunction, then, interferes with the aforementioned goals. If dysfunctional movement inhibits activities of daily living, it is essential to understand the underlying mechanisms of aberrant motor skills, as a means of mitigating movement dysfunction. The following will explore dysfunctional movement from a muscle imbalance paradigm, while considering two key approaches: the biomechanical model, and the neurological model (Page, Lardner, & Frank, 2010).
The genesis of dysfunctional movement can be understood by two prominent viewpoints: the structural perspective, and the functional perspective (Page et al., 2010). The structural paradigm is the oldest and most prominent between the two approaches; orthopedic medicine is heavily predicated on structural perspectives, and deeply rooted in anatomy and biomechanics (Page et al., 2010).
Indeed, many structural lesions (i.e., damage to physical structures within the body) lend themselves to such an approach; structures such as broken bones, torn tendons, and ligaments can be diagnosed through magnetic resonance imaging (MRI) and X-ray, followed by surgery, immobilization, and rehabilitation (Page et al., 2010). Such protocols are effective in the aforementioned instances. However, the structural approach has its limitations; Page et al. (2010) noted that diagnostic tests may return inconclusive results, and surgeries may not solve lesions. It is the functional approach, then, that may shed light on a seemingly elusive problem.
Vladimir Janda, a Czech Neurologist, defined functional pathology as impairment of the reflexes, which in turn, negatively affects structural and physiological function (Page et al., 2010). Such a paradigm shift from a traditional structural perspective, which considers symptoms of pain, allows room for the functional approach, which seeks the origin or source of the pathology/movement dysfunction (Page et al., 2010).
Often, the cause of the movement impairment is derived from a complex interaction of structures and systems (i.e., functional approach). Conversely, the structural approach encourages the professional to view muscle and joint function in a vacuum, by observing muscle action exclusively through origin and insertion, and movement generated relative to itself. In essence, the biomechanical model does not allow room to consider human movement as a whole (i.e., which PR clients require, and everyone else), and its relation to dysfunction and pain.
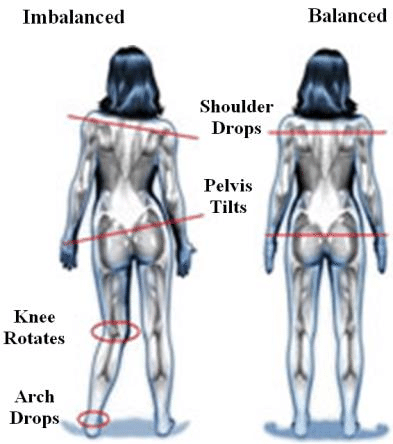
It is the contention of Page et al. (2010) that changes in normal human movement and pain finds its roots in muscle imbalances, both proximally and distally; an injured region can change its muscle balance and motor control immediately on and about (i.e., proximal) the injured tissue. Moreover, such a change can affect the behaviour of muscles and joint control further away (i.e., distal) (Page et al., 2010). In essence, seemingly unrelated regions of the body can influence each other, a concept in known as regional interdependence (Sueki, Cleland, & Wainner, 2013).
This is why it is paramount to consider that both proximal and distal faulty movement patterns can be implicated in the injured region. Muscle imbalance can be defined as a deviation in the length or strength of agonist and antagonist muscles, which alters normal function (Page et al., 2010). Two major forms of muscle imbalances can occur: functional and pathological. Functional muscle imbalances (FMI) are considered adaptive changes that occur to accommodate a particular movement pattern (Page et al., 2010). For example, baseball pitchers demonstrate a higher degree of external rotation in the throwing arm than the non-throwing arm. Such adaptive changes may help increase velocity of the baseball.
In general, FMI exhibits no pain, is not related to trauma, and is an adaptive change to accommodate a movement pattern (Page et al., 2010). Conversely, a pathological muscle imbalance (PMI) can impair function in its entirety, and is often associated with pain (i.e., most PR clients have this). Page et al. (2010) also noted that PMIs could come from a singular traumatic event, or slowly develop in an insidious fashion. In essence, FMI accommodates movement, while PMI inhibits movement. The following will consider two prominent models (i.e., biomechanical and neurological), which help explain mechanisms and solutions to mitigating muscle imbalances, movement dysfunction, and pain.
The biomechanical model asserts that muscle imbalances come from constant stresses that muscles experience from prolonged postures and repetitive movements. In turn, the aforementioned stresses and postures lead to adaptations in muscle stiffness, muscle weakness, as well as changes in muscle length (i.e., through adding sarcomeres in series) (Page et al., 2010). Such alterations negatively affect the role of synergists with respect to antagonists. Finally, alterations in normal muscle function by synergistic dominance leads to aberrant movement patterns, and abnormal stress on associated joints (Page et al., 2010).
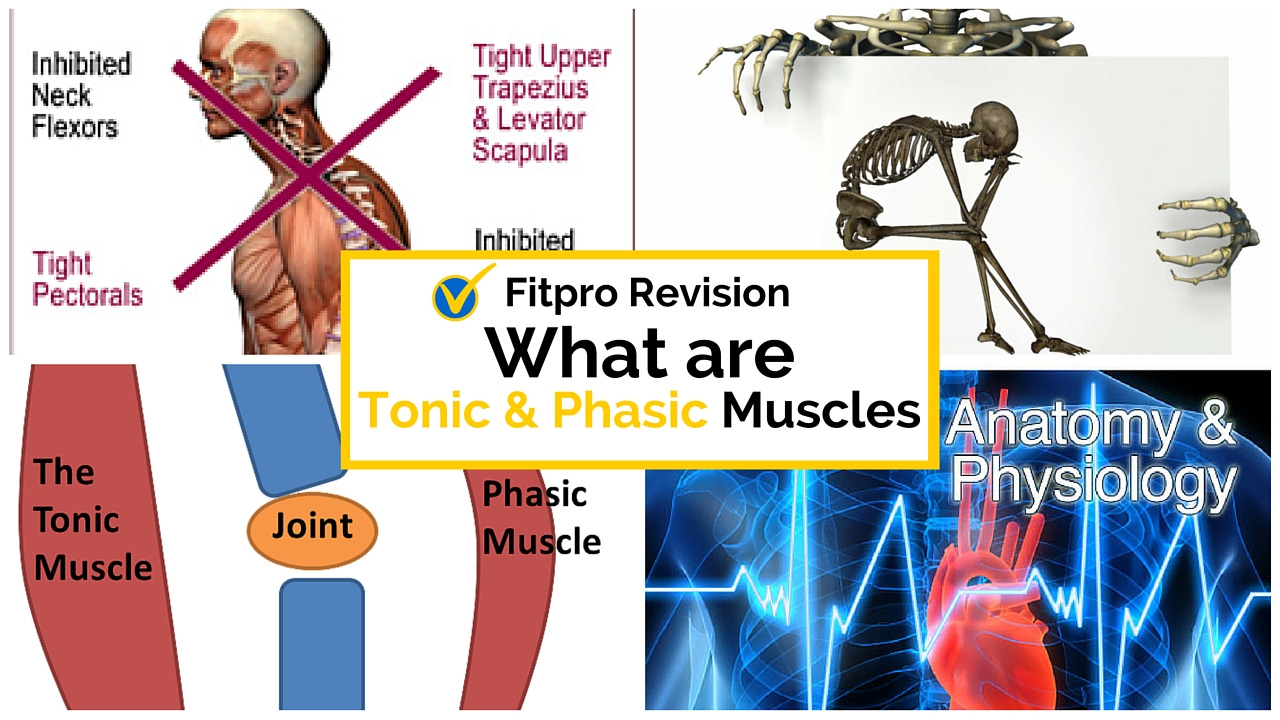
The neurological model argues that movement dysfunction is not structural (i.e., from prolonged postures/altered joint mechanics). Rather, movement impairment occurs because muscles are naturally predisposed to imbalance from a unique relationship to motor function (Page et al., 2010). Specifically, the neurological model postulates that muscle imbalance emanates from an impaired relationship between muscles that have a proclivity towards tightness (i.e., tonic), and those, which tend to become inhibited (i.e., phasic) (Page et al., 2010).
Vladimir Janda, an early proponent and progenitor of the neurological approach, believed that alternations in tonic and phasic muscles were driven by the nervous system. The neurological model submits that muscle imbalance is inevitable, and the central (CNS) and peripheral (PNS) nervous systems are responsible for maintaining proper muscle control, joint positions, and movement patterns through proprioceptive feedback and reflexes (Page et al., 2010). Having considered the role of the nervous system in dysfunctional movement, the following will explore the application of the neurological approach within the context of exercise.

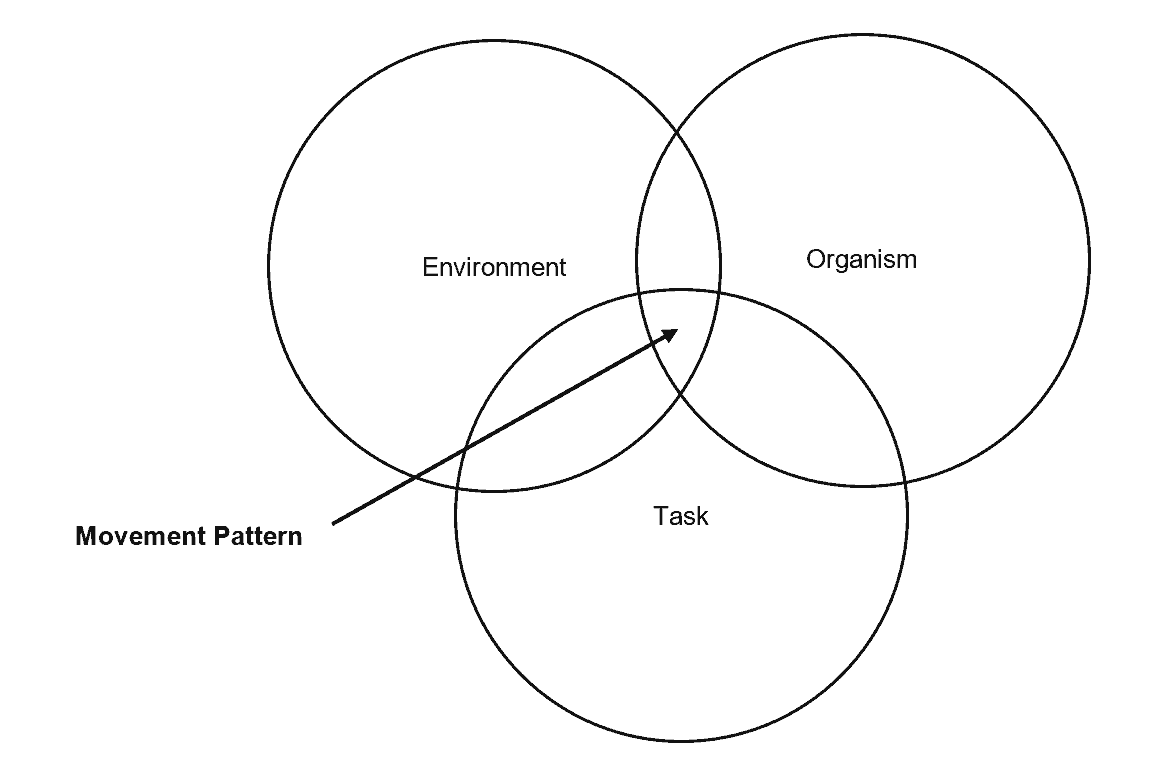
If movement is managed by the CNS and PNS, it would seem reasonable to re-train movement patterns from the neurological level. Such an approach can be implemented through the dynamic systems theory (DST). DST could be considered the tool, through which the neurological approach is applied; DST submits that movements are stimulated by and shaped through the interaction of the person (i.e., task constraint), movement goal (i.e., task constraint), and the surroundings (i.e., environmental constraint) (Magill, 2011).
Thus, DST can “feed” the proprioceptive inputs and reflexes found within the neurological approach. DST uses the aforementioned constraints as stimuli and information to develop and shape muscle and joint positions into meaningful and purposeful movements, similar to a funnel guiding water. Using the deadlift (i.e., an exercise that teaches individuals how to lift objects off the floor safely) as the example, the complex motion is shaped by having a client stand with knees directly in front of a bench (i.e., proprioceptive input).
As the client hip hinges, the only recourse is to drive the clients hips posteriorly (i.e., reaction) thereby inducing a hip hinge. If the client is having trouble maintaining a neutral spine during the hinge, a secondary task constraint, in the form of a dowel or broom handle, is placed along the entire spine. The client is instructed to keep the head and hips adjacent to the dowel. When the client loses contact, he/she knows (i.e., proprioceptive input) to re-adjust thereby inducing a neutral spine (i.e., reaction) during the hinge. In time, the client will move through the deadlift pattern with increased smoothness and efficiency, as the new movement pattern emerges, (a key characteristic of DST) (Magill, 2011). Once the client demonstrates movement competency, constraints are slowly removed.

It is finally at this stage that clients are ready to perform functional strength exercises (i.e., squatting, lifting, pushing, pulling, carrying, and locomotion) with competency and reduced risk of re-injury. It might also be stated that large robust motions are chosen for another reason besides their functionality; the body does not operate individual muscles. The body does, however, manage multiple joints and muscles all at once, in a harmonious and synchronized fashion. A concept known as coordinative structures states that the body organizes and coordinates particular groups of muscles to achieve an action goal (i.e., performing functional exercises) (Magill, 2011).
This is why, during post-rehabilitation, our goal is to introduce multiple forms of complex, functional exercise that challenges the neurological system, and its muscles. Although other exercise professionals may begin strength training immediately and finish quickly (i.e., 10-12 sessions), it might be fallacious and short-sighted to begin a PR client with strength exercises if there are deficits (almost always in my work) in postures, movement patterns, and motor control; my team of Kinesiologists and I screen each client for motor control and fundamental movement pattern deficits to help detect and reduce risks of injury. In conclusion, there is ample evidence that ignoring postures, movement patterns, and motor control can exacerbate the chronic musculoskeletal pain cycle, and hinder the productivity of a strengthening program (Page et al., 2010).
The aforementioned approaches encourages us to look beyond seemingly obvious regions exhibiting movement dysfunction; such a paradigm shift encourages one to consider the kinetic chain in its entirety, its involvement in faulty movement patterns, and the neurological drivers governing complex motions. Finally, such a methodology acknowledges and integrates the dynamic interplay of multiple systems, while providing an evidence-based approach and algorithm to screening, mitigating movement dysfunction, and strengthening the individual with robust, full body exercises.
It is my sincerest hope that the aforementioned sections have shed light and insight into the steps required return an individual back to prior function, under the supervision of a Kinesiologist. We may be a new profession, but we possess the capacity, knowledge, and professionalism to affect meaningful changes in the function and health of our clients. We believe in client-centered care, and we are here to help clients, help themselves. However, I hope that it is now clear why we require time, to reach that end.
References
Bron, C., Dommerholt, J., Stegenga, B., Wensing, M., & Oostendorp, R. A. B. (2011). High prevalence of shoulder girdle muscles with myofascial trigger points in patients with shoulder pain. BMC Musculoskeletal Disorders, 12, 139.
Cech, D., & Martin, S. (2012). Functional movement development across the life span (3rd ed.). St. Louis, MO: Elsevier Health Sciences.
Magill, R. A. (2011). Motor learning and control: Concepts and applications (9th ed.). New York: McGraw-Hill.
Page, P., Lardner, R., & Frank, C. (2010). Assessment and treatment of muscle imbalances: The Janda approach. Champaign, IL: Human Kinetics.
Sueki, D. G., Cleland, J. A., & Wainner, R. S. (2013). A regional interdependence model of musculoskeletal dysfunction: Research, mechanisms, and clinical implications. Journal of Manual and Manipulative Therapy, 21(2), 90-102.
-Michael McIsaac
