INTRODUCTION
Did you know that traumatic brain injury (TBI) affects over 69 million individuals globally, and is a prominent cause of long-term disability and death?1 Those are startling statistics. I work with a LOT of clients recovering from car accident injuries, and recently worked with an individual suffering from TBI. This inspired me to learn more about TBI, how it negatively affects the individual, and nutritional interventions to support recovery from TBI. Let’s learn a little more together in the following sections.
WHAT IS TBI EXACTLY?
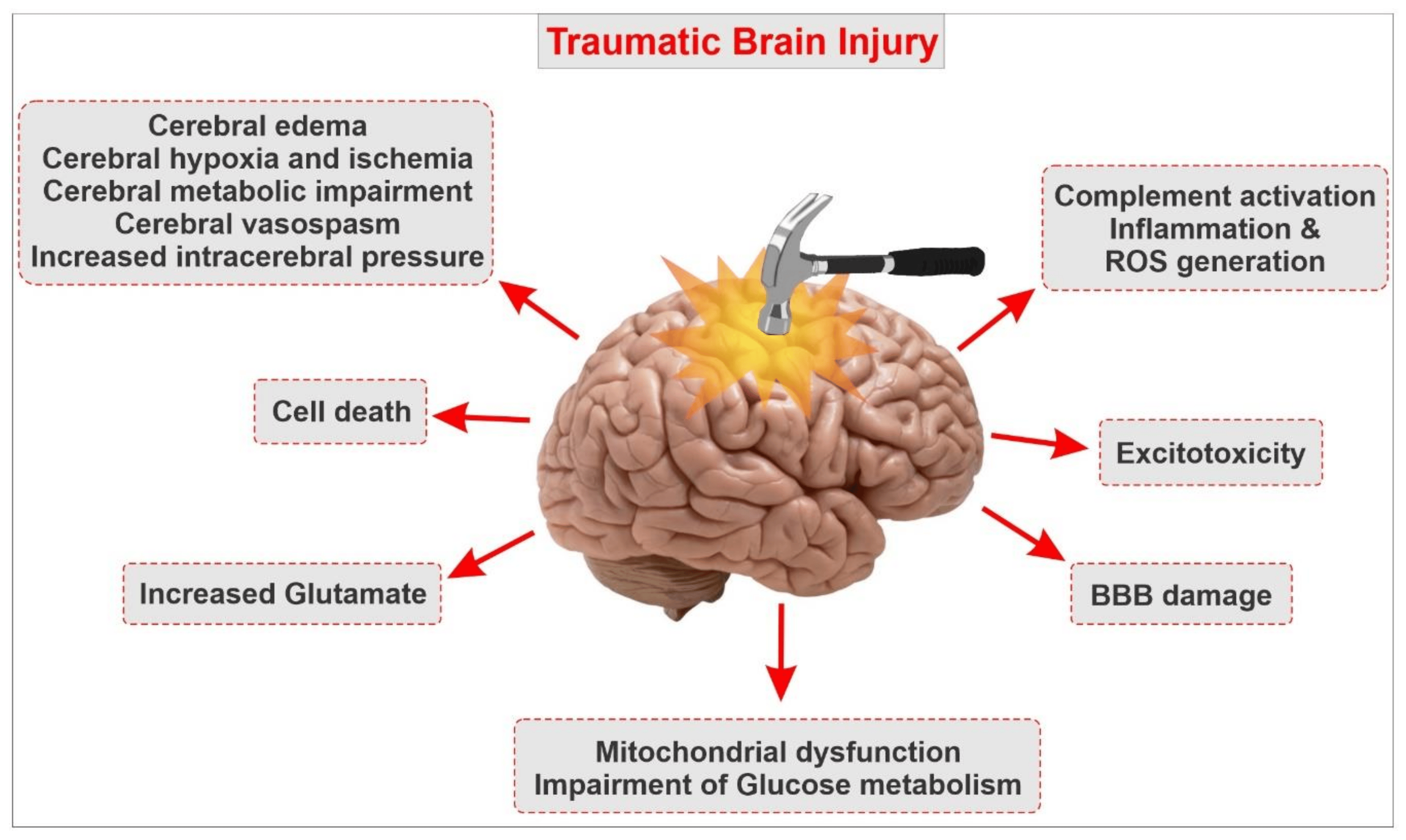
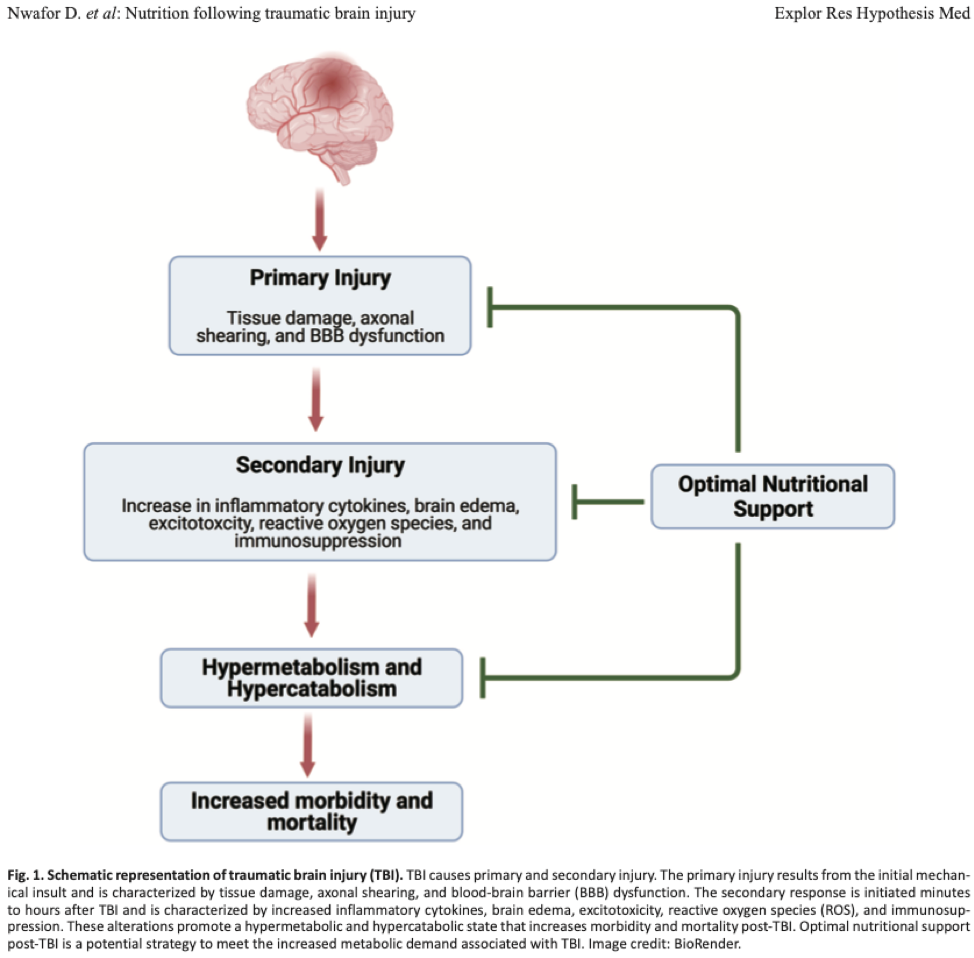
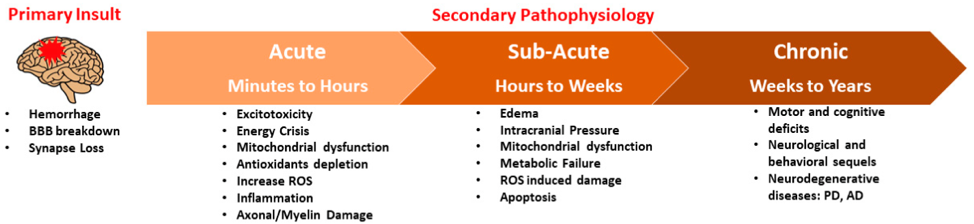
TBI is a form of structural damage, also known as a primary injury, to the central nervous system (CNS).2 Nwafor et al2(236) noted that primary injuries included:
- tissue deformation
- axonal shearing (i.e., destruction of the most basic units of the nervous system)
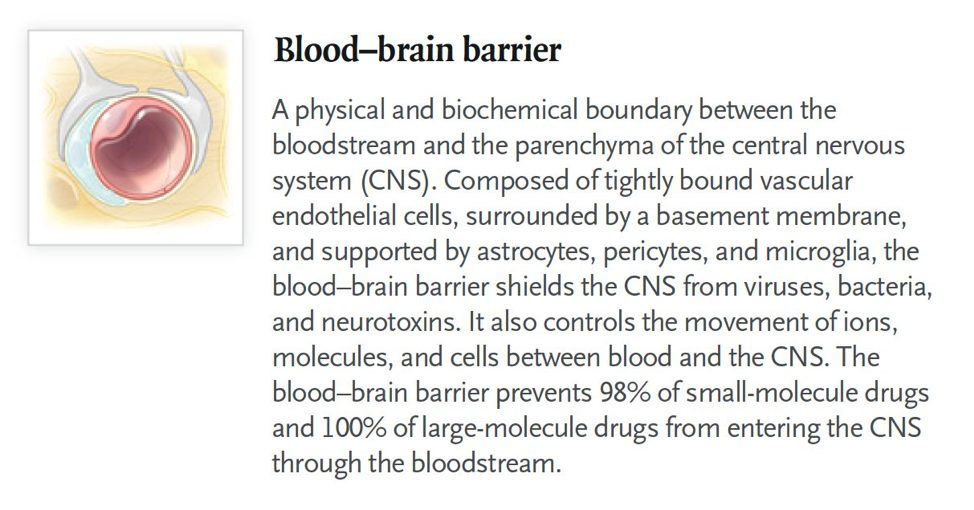
- dysfunction of the blood brain barrier (“separates” the brain and spinal cord from the rest of the body)
Other forms of injuries occur as a result of the primary injuries outlined above. These are termed secondary injuries by Nwafor et al2(236) to include:
- cerebral edema (i.e., swelling and excessive fluid buildup of the brain)
- immunosuppression (i.e., weakening of the immune system)
- increased reactive oxygen species (i.e., substances that break down cells and disrupt organ function)
- ischemia (i.e., restricted blood flow)
- excitotoxicity (i.e., excessive stimulation of CNS receptors, leading to nerve injury/death)
- increased presence of inflammatory cytokines (i.e., chemical messengers that drive inflammation)
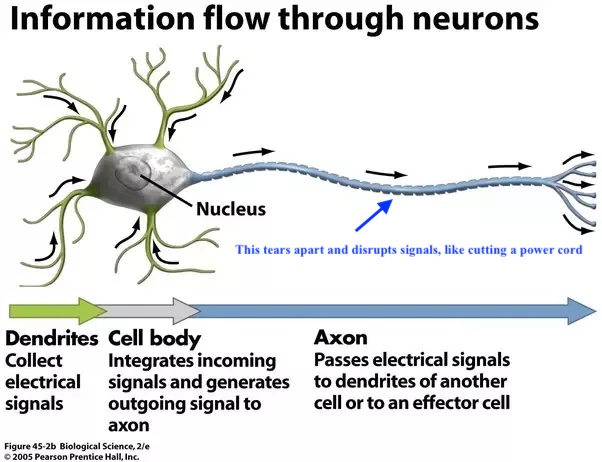
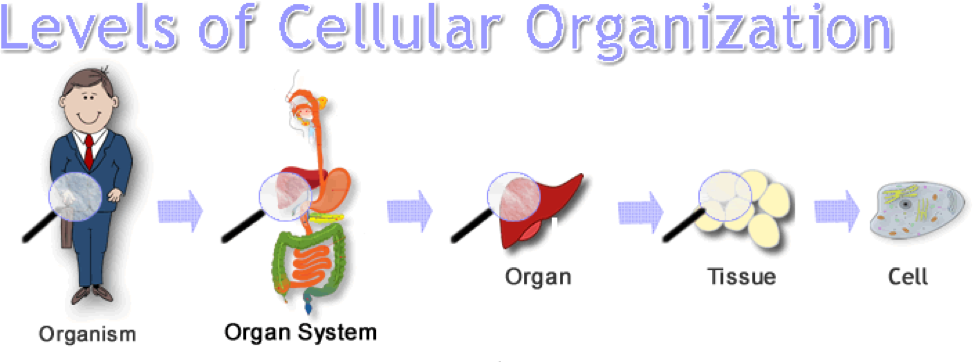
Primary and secondary injuries that occur with TBI eventually leads to dysregulation of the basic structures of the nervous system (cells).2(236) This in turn drives hypercatabolic (breakdown of cells and tissues in the body) and hypermetabolic (elevated resting energy use) states (more on these changes in a minute).2(237)
ARE THERE OTHER SYMPTOMS OF TBI?
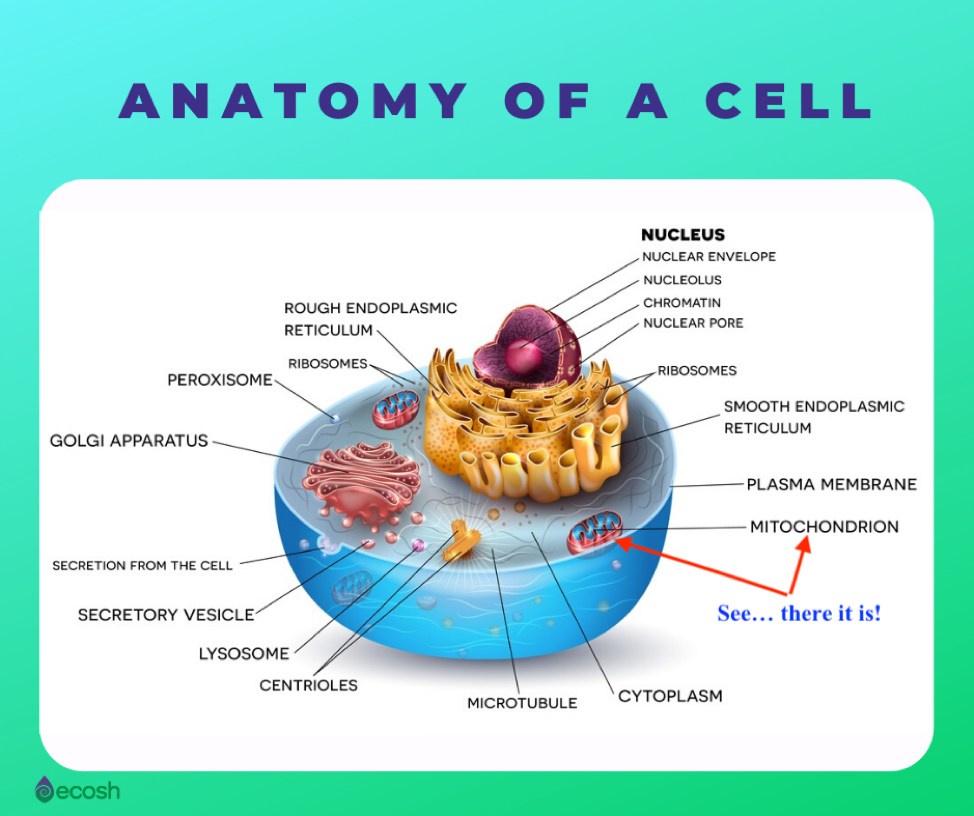
Admittedly, the primary and secondary injuries outlined above are often beginning at the cellular level. This can make it hard for us to appreciate how a TBI can affect us as an individual. But as you can see in the infographic above, cells make tissues, which makes organs, eventually leading to you as a person.
However, there are symptoms that can manifest and become noticeable to you depending on the severity of the TBI. Ryan et al3 stated that TBIs can be classified as mild, moderate, and severe:
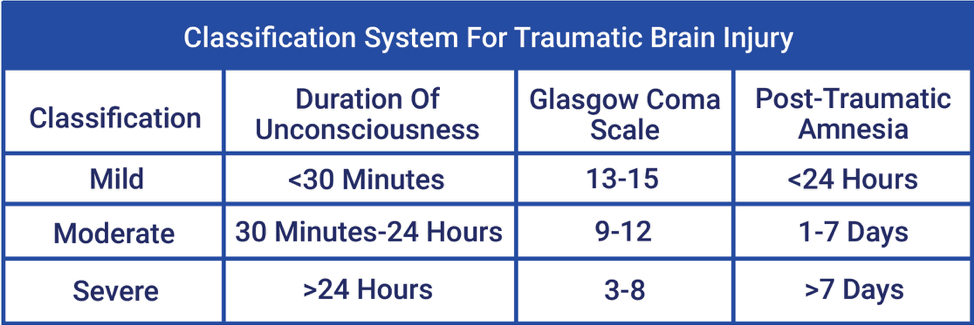
Mild
- loss of consciousness up to 30 minutes.3(2)
- amnesia for up to 24 hours.3(2)
- typically no skull fractures.3(2)
- headache.5
- nausea.5
- fatigue.5
- speech problems
- blurred vision.5
- ringing in ears.5
- light and sound sensitivity.5
- memory problems. 5
- mood swings. 5
- anxiety.5
- depression.5
- sleep disruptions.5
Moderate
- can include some or all of the symptoms of a mild TBI (mTBI).5
- amnesia up to 7 days.6
- loss of consciousness more than 30 minutes but less than 24 hours.4
- skull fractures present.3(2)
- persistent headaches that intensify.5
- repeated nausea.5
- convulsions.5
- dilation of on/both pupils.5
- clear fluids draining from the nose.5
- inability to wake up from sleep.5
- weakness/numbness in extremities.5
- loss of coordination.5
- deep confusion.5
- slurred speech.5
- agitation.5
- coma.5
Severe
- can include some or all of the symptoms of a mTBI.5
- loss of consciousness beyond 24 hours.4
- amnesia greater than 7 days.6
- skull fractures present.3(2)
- persistent headaches that intensify.5
- repeated nausea.5
- convulsions.5
- dilation of on/both pupils.5
- clear fluids draining from the nose.5
- inability to wake up from sleep.5
- weakness/numbness in extremities.5
- loss of coordination.5
- deep confusion.5
- slurred speech.5
- agitation.5
- coma.5
BEFORE WE GO DEEPER DOWN THE RABBIT HOLE
FYI, approximately 95% of people experience mTBI’s, and 75% of those individuals will have resolution of symptoms after about a month or so.3(2) However, symptoms can stick around negatively affecting an individual’s long-term health.3(2) Furthermore, repeated TBI’s are likely to compound said issues.

BACK TO THE CELL
Cells are the most basic functional unit of an organism.7 When enough of these are not working well, we do not work well. If an individual experiences a TBI, such as those seen in motor vehicle accidents, brain cells will experience unfavorable neurometabolic (means a problem with nerve cell processes to maintain life) changes.8 Some of these changes include:
- imbalances between cellular ions like sodium (NA+), potassium (K+), and calcium (Ca+) …these help nerve cells “communicate” with each other among other functions.8(2)
- too much Ca+ inside the cell (especially in the cell “generators” called the mitochondria) drives mitochondrial dysfunction, oxidative stress, neuroinflammation, and cell death.8(2)
- overproduction of free radicals causing oxidative stress, disrupts cell function.8(2)
- processes that produce cellular energy become disrupted.8(2)
- an imbalance between energy demand and supply become disrupted.8(2)
- the energy imbalance above drives high blood sugar (hyperglycemia) and protein catabolism (protein breakdown).8(2)
A LITTLE MORE ON THE IMMUNE RESPONSE
When a TBI happens, it is a good thing that oxidation and inflammation occur. These processes help repair damaged cells and tissues of the brain.8(2) However, these processes also demand “supplies” to do their job, to include anti-inflammatory and antioxidant nutrients.8(2) When the body does not have enough supplies (antioxidants and anti-inflammatory nutrients), deeper damage can happen such as:
- greater cellular metabolic disruption
- additional inflammation
- persisting TBI symptoms
- increased cell death
NICE REVIEW OF TBI. BUT HOW CAN I SUPPORT RECOVERY?
Finnegan et al8(2) stated that current mTBI protocols includes cognitive and physical rest for 1-2 days after the injury, as a means of reducing metabolic brain demands. Following rest, patients are encouraged to gently return to activities of daily living. Beyond this, there is not much more information available following these recommendations.8(2) However, there are preclinical (i.e., rat-based studies) and some human studies which explore how (i.e., mechanisms) nutritional interventions could support TBI recovery. The following will consider these in greater detail.
Interestingly, there is a large base of information and research (see below links) indicating the value of nutrition and lifestyle (i.e., optimal sleep, daily exercise, etc…) interventions for supporting other neurological issues and general neurological health. Although TBI-specific nutritional research is limited in human trials, research is emerging.8(2)
LINK: COLD WATER IMMERSION: IS IT WORTH DOING?
LINK: DEPRESSION: HOW DOES EXERCISE HELP?
LINK: TIME RESTRICTED FEEDING: A POTENTIAL PROTOCOL FOR MANAGING DEMENTIA
LINK: DEMENTIA: SUPPORT WITH SAUNA THERAPY
NUTRITION AND TBI SUPPORT: LOW CARBOHYDRATE DIETS
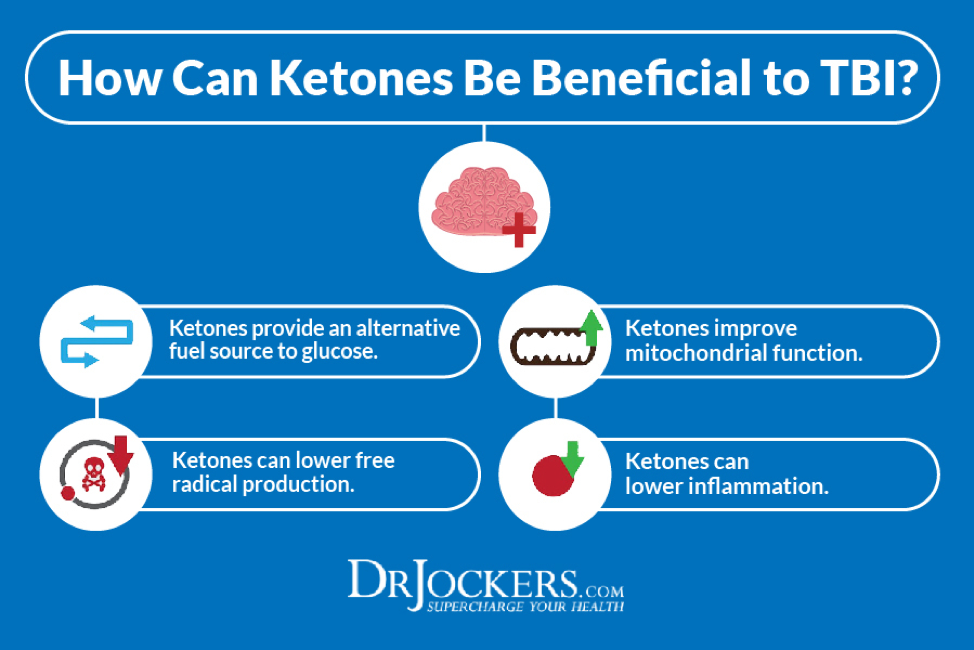
Did you know that energy demands from damaged brain cells increases to 100-200% compared to normal/pre-TBI energy use?1(2) That is a lot, and can last between a few weeks to several months.1(2) This gives us a hint that the brain and body are working hard to repair damaged tissue as much as possible. As noted in previous sections, one problem that TBI patients experience is hyperglycemia (high blood sugar). Having extra blood sugar (i.e., glucose) floating around can become problematic because it is associated with/causes oxidative stress, altered gene expression, cardiovascular disease, kidney disease, retinopathy, neuropathy, cancer, osteoarthritis, and weakened immunity… just to name a few.9 This process becomes further complicated by increases in insulin production and secretion to help manage hyperglycemia; a process known as hyperinsulinemia.10
If the body is managing glucose levels poorly, gently lowering glucose consumption (processed foods, carbohydrate-rich foods) can help stabilize blood sugar by causing the body to produce energy from other sources; a process known as ketogenesis, and one that can help resolve many of the complications of hyperglycemia. Finally, this process helps individuals avoid producing and/or taking extra insulin, which can drive deeper energy crisis’s in the brain tissue.1(7) I have written about low carbohydrate diets and their health benefits in other articles. Please see links below:
LINK: INSULIN REISTANCE, TYPE 2 DIABETES, AND CARBOHYDRATE RESTRICTION
LINK: HYPERINSULINEMIA, TYPE 2 DIABETES, AND LOW CARBOHYDRATE NUTRITIONAL INTERVENTIONS
LINK: HYPERINSULINEMIA: AN EARLY WARNING TO TYPE 2 DIABETES
LINK: HYPERINSULINEMIA, PRE-DIABETES, AND EARLY DETECTION
LINK: KETOGENIC DIETS AND BRAIN CANCER
LINK: BENEFITS OF VERY LOW CARBOHYDRATE DIETS
LINK: LOW CARBOHYDRATE NUTRITION: MANAGING HIGH TRIGLYCERIDES AND LOW-DENSITY LIPOPROTEINS
LINK: LOW CARBOHYDRSATE DIETS, GRAIN DIETS, AND BIOMARKERS
LINK: METABOLIC SYNDROME, DIABETES, AND LOW CARBOHYDRATE DIETS; EXPLORING THE CONNECTION
LINK: LOW CARB DIETS AND METABOLIC SYNDROME: CAN THEY OPTIMAIZE HEALTH?

NUTRITION AND TBI SUPPORT: OPTIMAL PROTEIN INTAKE
As we now know, another major change that the brain initiates during TBI is increased catabolism (protein breakdown in the body). This is a way for the brain to access amino acids (the little parts that make up protein) from other parts of the body for repair. This is also a very important process because amino acids are the most critical nutrient for the recovery of brain damage.1(7)
However, catabolism (muscle breakdown for amino acids) can lead to muscle tissue loss (where amino acids are found in abundance). The good news is that if enough protein is supplied through the diet, catabolism can be better managed.8(20) Optimal daily protein requirements, especially during the few days of a TBI, is suggested to be 1.2-2.0 g/kg body weight.1(8)
LINK: ESSENTIAL AMINO ACIDS AND WHY THEY MATTER
LINK: PROTEIN AND BONE HEALING
LINK: ASSESSING HEALTH THROUGH PROTEIN STATUS
LINK: PROTEIN AND SATIETY
LINK: THE ELDERLY: OPTIMAL PROTEIN CONSUMPTION AND BEST SOURCES
NUTRITION AND TBI SUPPORT: OMEGA-3 FATTY ACIDS
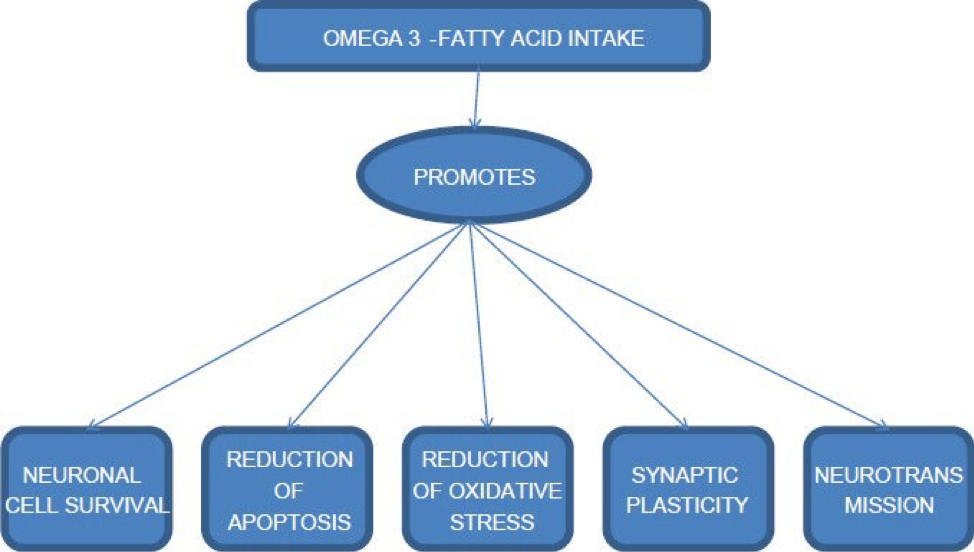
Research is limited in human trials, but animal research has suggested potential benefits of omega-3 fatty acids (O3FAs); rats with TBI who were supplemented with O3FAs, compared to rats with TBI who did not supplement with O3FAs, had noticeable improvements in cognition and sensorimotor tasks.11
This matters because O3FAs are lower in TBI brain tissue compared to brain tissue without TBI.11(121) Furthermore, it is well understood that O3FAs help form the membrane wall of nerve cells; O3FAs come in two forms known as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).11(121) DHA is the main fatty acid that forms these nerve cell walls.
When nerve cells are abundant with DHA, you will see improvements in axonal and dendritic stability (a part of a nerve cell…see image earlier in this article), neuroinflammation, hypothalamic (regulates many body functions) processes, glucose uptake (manages hyperglycemia), and neuronal plasticity (fancy way of describing the capacity to learn, develop and form memories etc…).11(121)
Interestingly, there are other reasons to provide an abundance of O3FAs during a TBI; when brain injury occurs, the blood brain barrier (BBB) lowers the entry of anti-inflammatory pharmacological agents (we spoke earlier about how critical it is to control inflammation).13 However, the BBB does indeed permit entry of O3FAs, providing at least one method of helping control the inflammatory cascade.13(599)
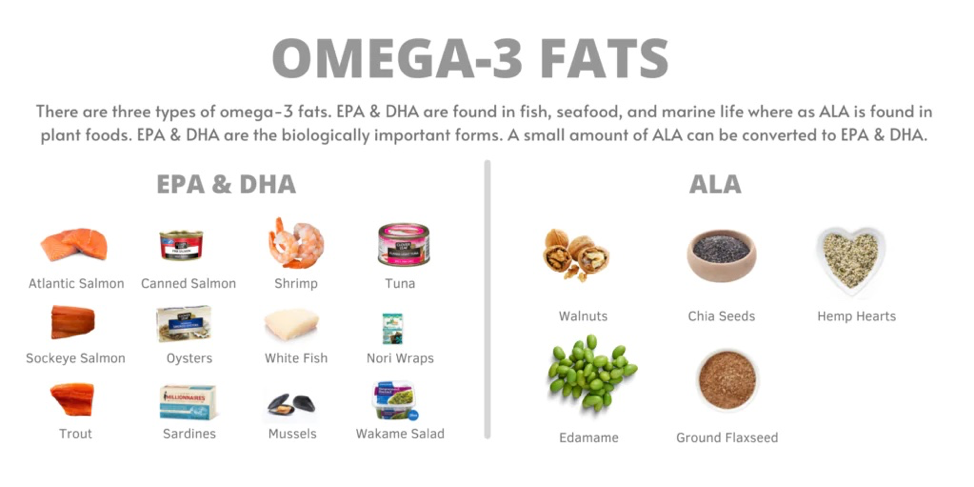
You might be wondering how much O3FAs you should take each day. Research suggests that as much as 5000 mg of EPA/DHA per day poses no safety concerns in adults.12 For individuals that are interested in uncovering their blood levels of O3FAs, there is a simple home-based test known as the omega-3 index test.14
LINK: OMEGA-3 INDEX TEST
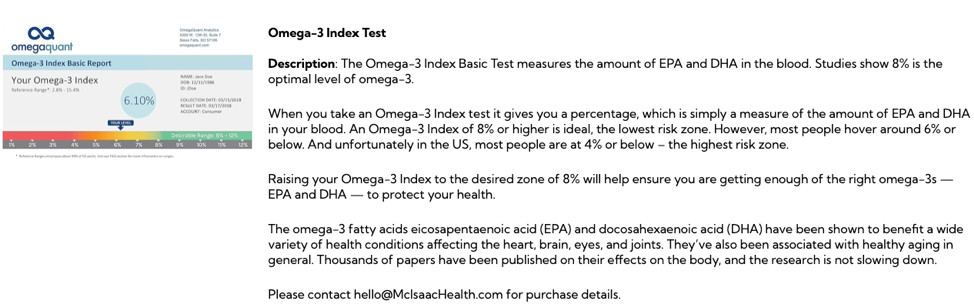
This test helps you reach optimal levels in your body. Cell membranes need to work well in order to keep you healthy. Part of that process is having enough polyunsaturated fatty acids in the membrane; healthy cells have at least 8% of their membranes composed of O3FAs, and that number is also associated with a cardioprotective effect and a decreased risk of sudden death.14(4)
Please see additional links below to uncover the widespread benefits of having O3FAs in your diet:
LINK: OMEGA-3 SUPPLEMENTATION: SUPPORTING RESISTANCE TRAINING AND RECOVERY
LINK: INFLAMMATION, CORONARY ARTERY DISEASE, AND OMEGA-3 FATTY ACIDS
LINK: METABOLIC SYNDROME, LOW-DENSITY LIPOPROTEINS, AND FISH OIL
LINK: KRILL OIL VS FISH OIL
LINK: NON-ALCOHOLIC FATTY LIVER DISEASE: SUPPORT WITH OMEGA-3 FATTY ACIDS

NUTRITION AND TBI SUPPORT: ANTIOXIDANTS
Earlier in this article, I mentioned that TBI causes dysregulation within nerve cells to include uncontrolled oxidation/oxidative stress. When cells make energy (specifically within the mitochondria), by-products known as free radicals are produced; they are like exhaust from your car engine.15
LINK: MITOCHONDRIA AND RELATIONSHIPS TO HEALTH
Healthy mitochondria have an abundance of substances known as antioxidants. Antioxidants, when at optimal levels in the body, help prevent damage (i.e., oxidative damage) that free radicals could produce. This is achieved by antioxidants “giving” the free radicals/reactive oxygen species (ROS) what it is seeking (i.e., electrons).
LINK: ANTIOXIDANTS AND CELL HEALTH
When this process occurs, cells and the parts inside of cells, remain undamaged/less damaged.15(3) However, damaged brain cells from TBIs change this process, and an overabundance of free radicals/ROS can occur within minutes after a head injury.15(3) The imbalance between free radicals/ROS and antioxidant supply is known as oxidative stress.16
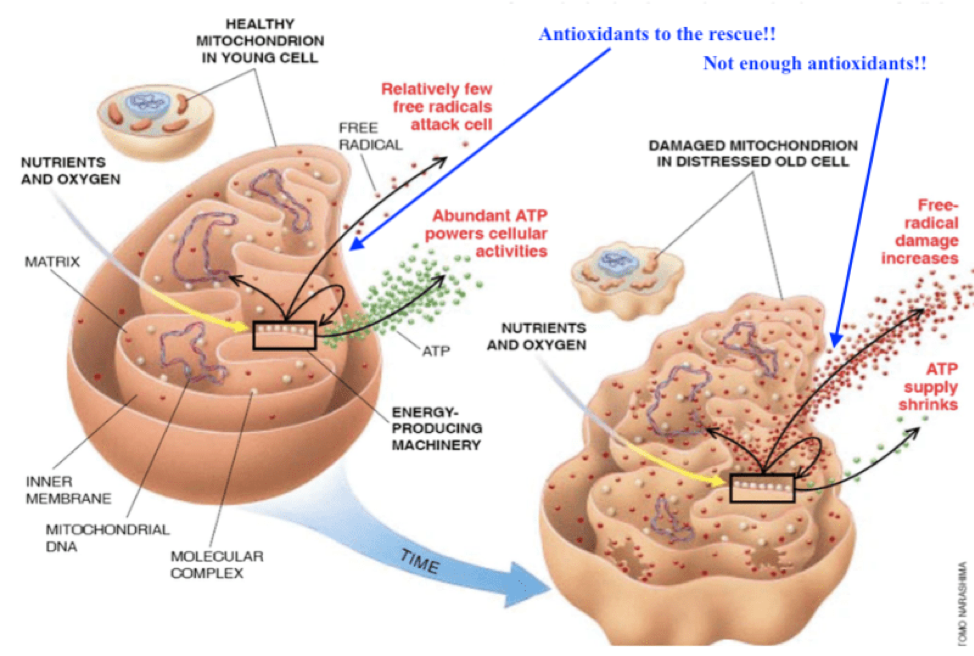
If free radicals and ROS go unchecked and are not properly neutralized, they can disrupt the functioning of other cell components (fancy term is organelles) such as proteins, lipids, and DNA.15(3) This process is termed oxidative damage.15(5) The good news is that there are interventions to help manage this.
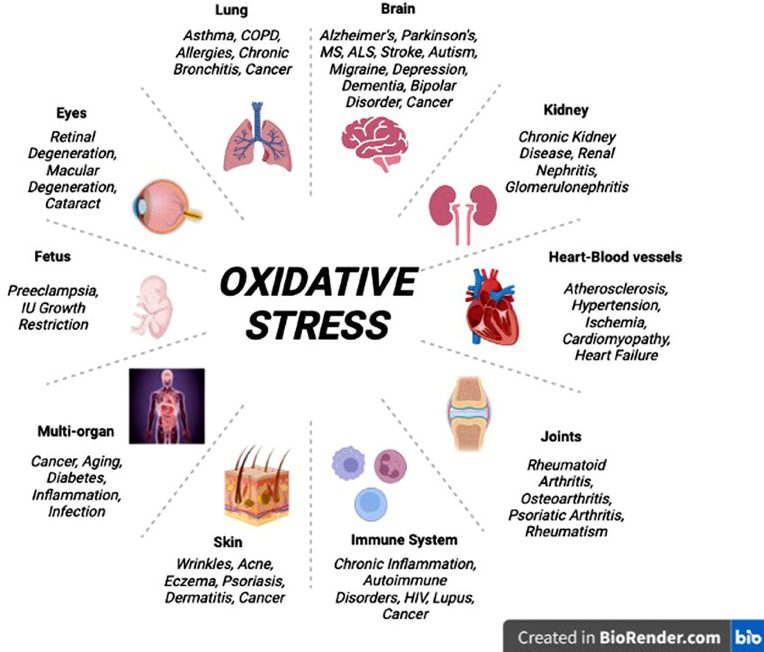
As you can see in the image above, oxidative stress can affect MANY parts of your body.
The good news is that antioxidants are easily found in many foods. If you are wondering, antioxidants/antioxidant precursors include, but are not limited to:
- vitamin A.15(7)
- vitamin E.15(7)
- vitamin C.15(7)
- coenzyme Q10.15(7)
- carotenoids.15(7)
- polyphenols.15(7)
- flavonoids.15(7)
- copper.15(7)
- zinc.15(7)
- selenium.15(7)
- alliin/allicin.15(7)
LINK: ANTIOXIDANTS AND TRACKING OXIDATIVE STRESS
** Feel free to search the above antioxidants on McIsaacHealth.com for more information**

FYI, there are a set of tests that can assess the degrees of oxidative stress and inflammation in your body so you can uncover the extent of cell/organ damage you might be experiencing. These tests can also provide insights on your levels of antioxidants, among other vital micronutrients (vitamins, minerals, trace elements) and macronutrients (amino acids, fatty acids) that keep you healthy. Knowing your levels can help you better determine how much antioxidant-rich foods you are consuming, in addition to considering supplementation when and where indicated. NutraEval tests can provide this opportunity to you. Please see the link and image below:
LINK: NUTRAEVAL

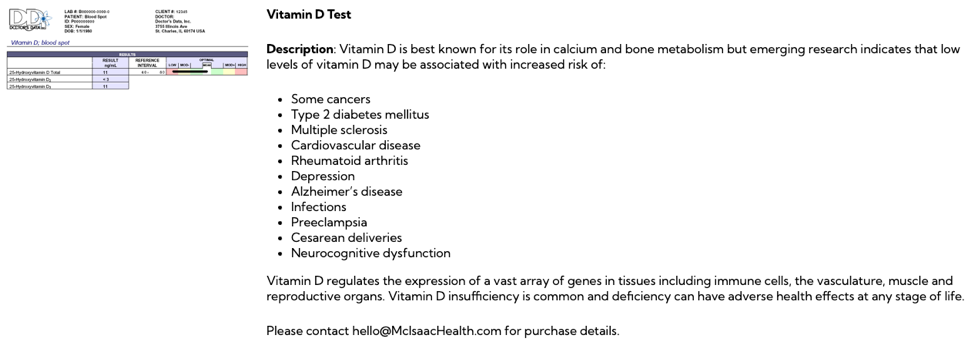
NUTRITION AND TBI SUPPORT: VITAMIN D3
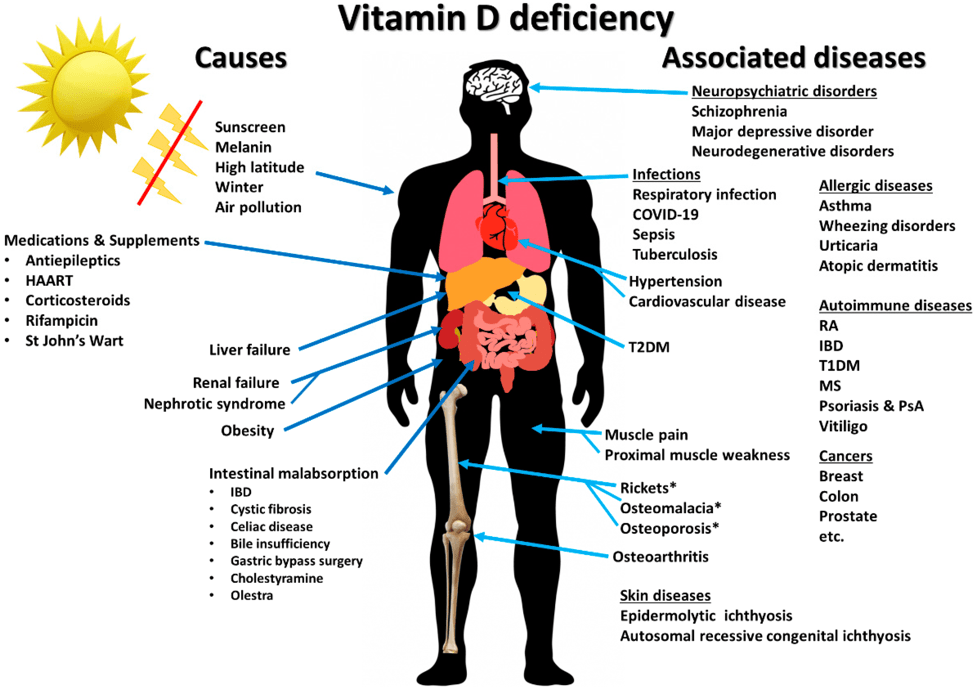
Last, but certainly not least, is consideration of optimal vitamin D3 (VD3) levels in the body. Did you know that almost every cell in the human body has vitamin D receptors?17 That should be a little hint about how important vitamin D is to each cell, and you. Vitamin D is mostly known for its roles in helping support the development and maintenance of strong bones. However, vitamin D’s role extends far beyond bone metabolism.17(1)
Please see the links below for more information on vitamin D’s widespread roles:
LINK: DETERMING OPTIMAL VITAMIN D LEVELS
LINK: VITAMIN D: TYPES, UTILITY, SCREENING, AND OPTIMAL DOSING
LINK: VITAMIN D3 PRODUCTION
LINK: VITAMIN D SUPPLEMENTATION: WHEN, HOW, AND WHY?
LINK: VITAMIN D AND HIDDEN HUNGER
LINK: MULTIPLE SCHLEROSIS, NEUROLOGICAL SUPPORT, AND VITAMIN D3
LINK: VITAMIN D AND THE COMMON COLD
LINK: VITAMIN D3 AND CROHN’S DISEASE
LINK: CROHN’S DISEASE, VITAMIN D, AND SINGLE NUCOLEOTIDE POLYMORPHISMS
LINK: VITAMIN D3 AND GUT INFLAMMATION
LINK: VITAMIN D SUPPORT FOR BREAST CANCER
LINK: ASTHMA: MANAGEMENT WITH VITAMIN D
LINK: ESSENTIAL HYPERTENSION: HOW VITAMIN D CAN HELP
LINK: VITAMIN D3 AND PROSTATE CANCER
LINK: VITAMIN D AND PRE-DIABETES: MANAGEMENT AND PREVENTION
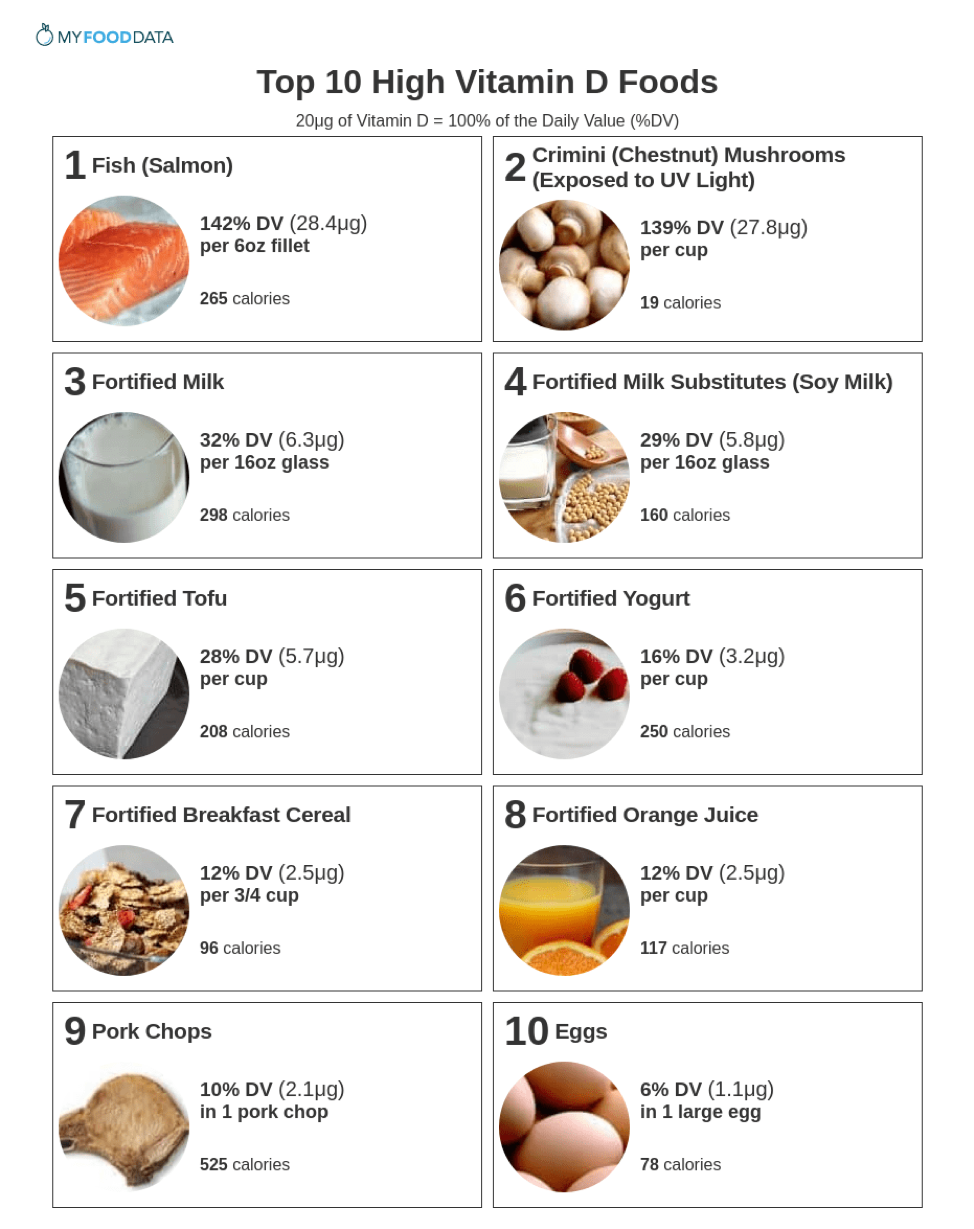
As I hope you can see, vitamin D has far reaching influence upon the human body. The challenge is, most people in the Northern hemisphere (i.e., Canada) are not receiving enough sunlight (and intensity of sunlight) throughout the year; a primary means of improving blood vitamin D levels.18 The good news is that food-based sources of vitamin D exist and can help get your levels up. However, you would have to eat a LOT of these foods to reach optimal levels of vitamin d in the blood. Considering, most people are quite deficient in Northern regions, supplementation of vitamin D3 (a form that is readily absorbable and usable) is quite reasonable.
The question you might be considering is how much vitamin D should be supplemented? One suggestion is to consume 1000 IU of vitamin D3 for approximately every 35 pounds of bodyweight (to a max of 4000 IU/day- because it is the official safe upper limit.19 There is a notion in the medical community that hypercalcemia (very high levels of calcium = dangerous) can occur if vitamin D supplementation exceeds 4000 IU/day. However, systematic reviews and meta-analysis of 32 randomized clinical trials in 8400 children aged 0-6 years indicated no increased risk of adverse events with doses as high as 10,000 IU vitamin D3/day.20
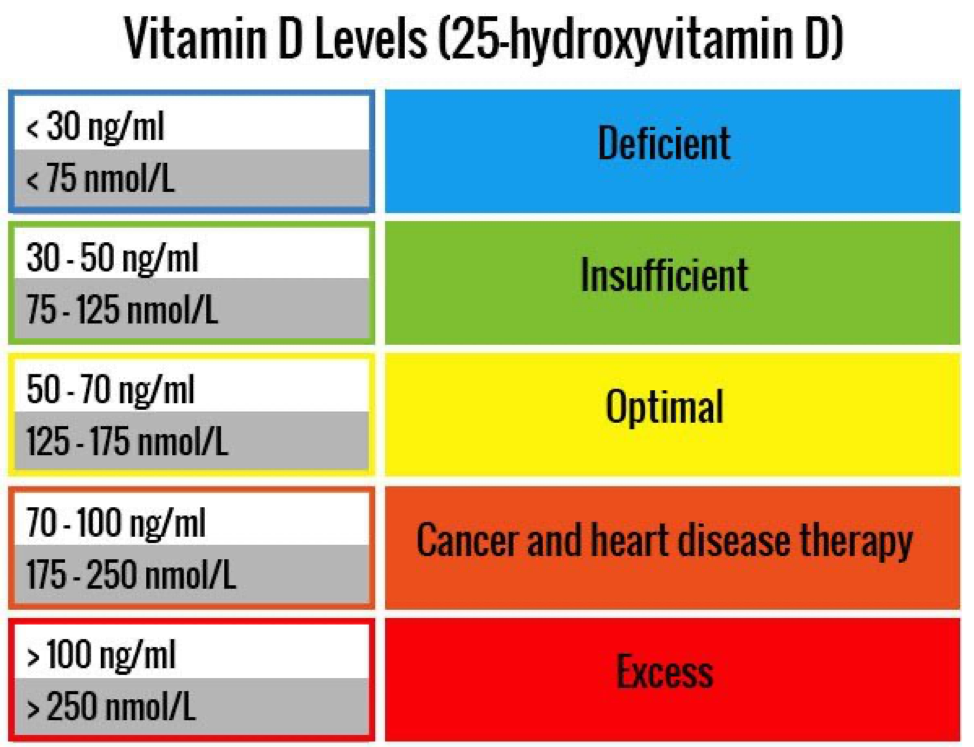
So, I would suggest up to 4000 IU of vitamin D3/day for about 3 months. At that point, you can purchase a home-based blood test (finger prick) that can tell you your levels. Optimal levels are likely somewhere between 50-70 ng/ml; a level commonly found among individuals living in sun-rich environments.21 See the link below for more on home-based vitamin D tests:
LINK: VITAMIN D TEST
MORE ON VITAMIN D AND TBI
Vitamin D has been known to support brain health through several key processes. Some of these include:
- regulating inflammation.22
- supporting optimal immune function.22(535)
- protecting neurons through detoxification, antioxidant, and nerve conduction mechanisms.22(535)
- increasing free radical scavenging. 22(537)
- improving vasodilation (i.e., improves blood flow) .22(535)
- decreasing blood pressure.22(535)
- regulating cell growth and cell death.22(535)
- stimulating nerve growth.22(535)
- decreasing glutamate release (decreases neurotoxicity). 22(537)
- improving BBB function.22(537)
- reducing brain edema (i.e., swelling).22(538)
As you can see, optimal vitamin D levels are beneficial for several organs in the body, to include the brain/nervous system. So consider getting out in the sun, look for signs/symptoms of vitamin D deficiency, check your vitamin D blood levels, and consider supplementation if necessary.
SUMMARY
- reduce processed foods/carbohydrates
- increase protein
- increase omega-3 fatty acids
- increase antioxidants
- increase vitamin D3

CONCLUSIONS
TBI is more common that we realize, and can truly affect an individual’s health, quality of life, and length of life itself. If you or somebody you know has experienced a TBI, please consider sharing this article. TBI is serious condition and I strongly encourage others to work very closely with their family doctor before considering the recommendations I outlined above. It is my hope that employing the above interventions, as part of a larger and more robust protocol overseen by medical professionals, will help support a full and successful recovery from TBIs.
References
1. Lee HY, Oh BM. Nutrition management in patients with traumatic brain nnjury:
A narrative review. Brain Neurorehabil. 2022;15(1) :1-14. doi:https://doi.org/10.12786/bn.2022.15.e4.
2. Nwafor D, Goeckeritz J, Hasanpour Z, Davidson C, Lucke-Wold B. Nutritional support for traumatic brain injury: A comprehensive review. Explor Res Hypothesis Med. 2023;8(3):236–247. doi:10.14218/ERHM.2022.00086.
3. Ryan T, Nagle S, Daly E, Pearce AJ, Ryan L. A potential role exists for nutritional interventions in the chronic phase of mild traumatic brain injury, concussion and sports-related concussion: A systematic review.Nutrients. 2023;15(17):1-33. doi:10.3390/nu15173726.
4. Cleveland Clinic Website. https://my.clevelandclinic.org/health/diseases/8874-traumatic-brain-injury. Updated January 24, 2024. Accessed July 28, 2024.
5. Mayo Clinic Website. https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/symptoms-causes/syc-20378557. Updated February 4, 2021. Accessed July 26, 2024.
6. Agoston DV, Elsayed M. Serum-based protein biomarkers in blast-induced traumatic brain injury spectrum disorder. Front Neurol. 2012;3(107):1-10. doi: 10.3389/fneur.2012.00107.
7. Reisner EG, Reisner HM. An Introduction to Human Disease: Pathology and Pathophysiology Correlations. 10thed. Burlington, MA: Jones & Bartlett Learning; 2017.
8. Finnegan E, Daly E, Pearce AJ, Ryan L. Nutritional interventions to support acute mTBI recovery.Front Nutr. 2022;9:1-26. doi:10.3389/fnut.2022.977728.
9. Giri B, Dey S, Das T, Sarkar M, Banerjee J, Dash SK. Chronic hyperglycemia mediated physiological alteration and metabolic distortion leads to organ dysfunction, infection, cancer progression and other pathophysiological consequences: An update on glucose toxicity.Biomed Pharmacother. 2018;107:306-328. doi:10.1016/j.biopha.2018.07.157.
10. Lee RD, Nieman, DC. Nutritional assessment. 6thed. New York, NY: McGraw-Hill. 2013.
11. Gupta A, Summerville G, Senter C. Treatment of acute sports-related concussion.Curr Rev Musculoskelet Med. 2019;12(2):117-123. doi:10.1007/s12178-019-09545-7.
12. Poblete RA, Yaceczko S, Aliakbar R, et al. Optimization of nutrition after brain injury: Mechanistic and therapeutic considerations.Biomedicines. 2023;11(9):1-25. doi:10.3390/biomedicines11092551.
13. Bailes JE, Abusuwwa R, Arshad M, et al. Omega-3 fatty acid supplementation in severe brain trauma: case for a large multicenter trial.J Neurosurg. 2020;133(2):598-602. doi:10.3171/2020.3.JNS20183
14. Harris WS. Omega-3 fatty acids and cardiovascular disease: a case for omega-3 index as a new risk factor.Pharmacol Res. 2007;55(3):217-223. doi:10.1016/j.phrs.2007.01.013.
15. Modi HR, Musyaju S, Ratcliffe M, Shear DA, Scultetus AH, Pandya JD. Mitochondria-targeted antioxidant therapeutics for traumatic brain injury.Antioxidants. 2024; 13(3):303. https://doi.org/10.3390/antiox13030303.
16. Cleveland Clinic Website. https://my.clevelandclinic.org/health/articles/oxidative-stress. Updated February 29, 2024. Accessed August 3, 2024.
17. Bikle DD. Extraskeletal actions of vitamin D.Ann N Y Acad Sci. 2016;1376(1):29-52. doi:10.1111/nyas.13219.
18. Chaplin G, Jablonski NG. The human environment and the vitamin D compromise: Scotland as a case study in human biocultural adaptation and disease susceptibility.Hum Biol. 2013;85(4):529-552. doi:10.3378/027.085.0402.
19. Cannell JJ, Hollis BW. Use of vitamin D in clinical practice.Altern Med Rev. 2008;13(1):6-20.
20. Brustad N,Yousef S, Stokholm J, Bønnelykke K, Bisgaard H, Chawes BL. Safety of high-dose vitamin d supplementation among children aged 0 to 6 years: A systematic review and meta-analysis. JAMA Netw Open.2022;5(4):1-10. doi:10.1001/jamanetworkopen.2022.7410.
21. Rosen CJ. Vitamin D Insufficiency. N Engl J Med. 2011;364(3):248-254. doi: 10.1056/NEJMcp1009570.
22. Saadatmand K, Khan S, Hassan Q, et al. Benefits of vitamin D supplementation to attenuate TBI secondary injury?Transl Neurosci. 2021;12(1):533-544. doi:10.1515/tnsci-2020-0195.
-Michael McIsaac

